Pheochromocytoma – What It Is and Why It Matters
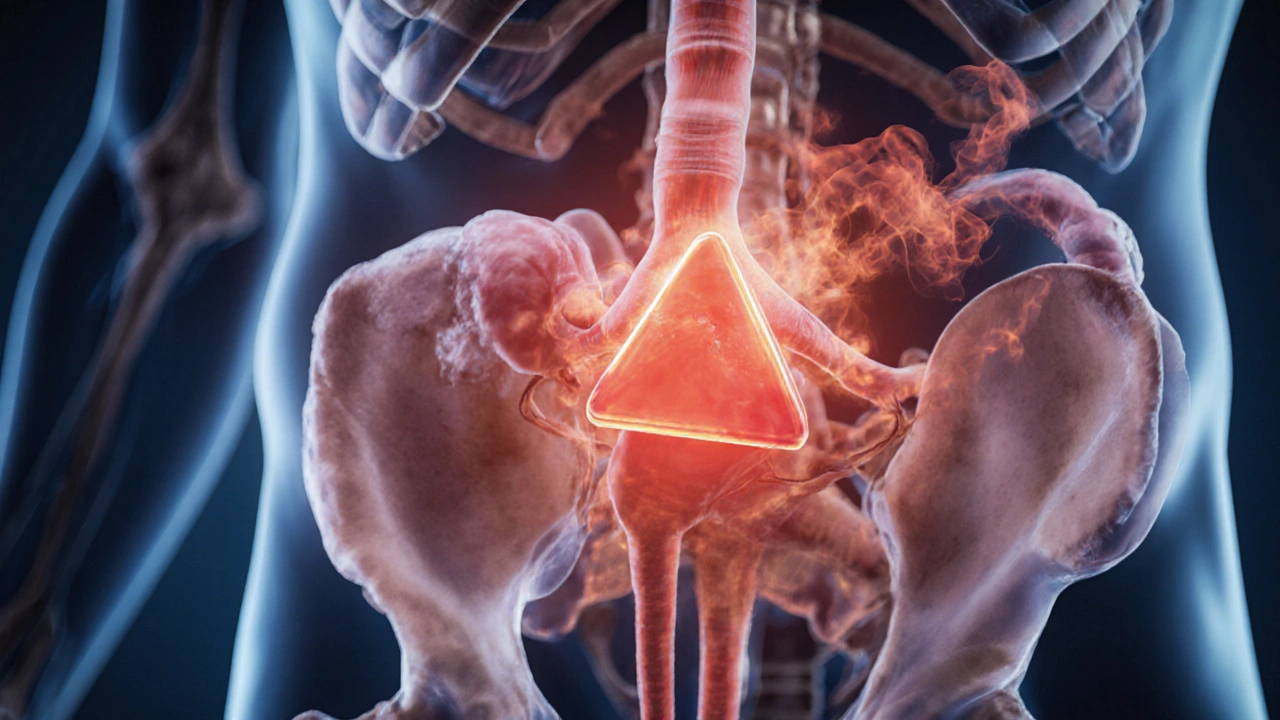
When dealing with Pheochromocytoma, a rare tumor that arises from the adrenal medulla and releases excess catecholamines. Also known as adrenal medullary tumor, it can cause sudden spikes in blood pressure and a range of other symptoms. Understanding this condition starts with knowing its main players.
The primary organ involved is the adrenal gland, specifically the inner medulla where the tumor forms. The gland normally produces catecholamine, a hormone like adrenaline that controls the "fight‑or‑flight" response. In pheochromocytoma, these hormones surge, leading to episodic hypertension dangerously high blood pressure that can swing up and down quickly. This link between tumor, hormone, and blood pressure is a classic semantic triple: Pheochromocytoma → produces → catecholamines → causes → hypertension. Because the excess hormones also affect heart rate, sweating, and anxiety, patients often describe a "panic attack" feeling that isn’t triggered by stress.
Genetics, Diagnosis, and Treatment Pathways
For many, the story begins with genetics. About 30% of cases are tied to hereditary syndromes such as MEN2 syndrome, a condition that also raises the risk of medullary thyroid cancer and other endocrine tumors. Knowing this relationship helps doctors decide when to screen family members – a clear example of the triple: MEN2 syndrome → increases risk of → pheochromocytoma.
Diagnosing the tumor hinges on measuring catecholamine levels in blood or urine. Imaging studies like CT or MRI then locate the growth within the adrenal gland. Together, lab tests and imaging create another semantic link: Diagnosis requires → catecholamine measurement + imaging. Once confirmed, the standard treatment is surgical removal of the tumor, often done laparoscopically. Pre‑operative medication to block the effects of catecholamines (alpha‑blockers first, then beta‑blockers) is essential to keep blood pressure stable during surgery. This procedural chain – Surgery requires → pre‑operative alpha‑blockade – reflects the practical steps patients face.
Even after surgery, follow‑up matters. Some patients develop recurrent disease or experience residual hypertension, so lifelong monitoring of blood pressure and periodic catecholamine testing are recommended. Lifestyle tweaks, like reducing caffeine and avoiding stress triggers, can also help keep symptoms at bay.
Below you’ll find a curated selection of articles that dive deeper into each of these areas – from the science behind hormone spikes to step‑by‑step guides on managing blood pressure and preparing for surgery. Whether you’re a patient, a family member, or a health‑care professional, the resources ahead give you practical, up‑to‑date information on living with and treating pheochromocytoma.
Pheochromocytoma & Exercise: Essential Safety Guidelines
Learn how to exercise safely with pheochromocytoma, covering medical prep, activity guidelines, red‑flag symptoms, and post‑surgery tips.
Read more