When your breathing stops repeatedly during sleep, your body doesn’t just feel tired the next day-it’s under real stress. Sleep apnea isn’t just snoring. It’s a condition where your airway collapses, cutting off oxygen, straining your heart, and raising your risk of stroke, high blood pressure, and even sudden death. For many, the solution isn’t a pill or surgery. It’s a machine that blows air into your nose while you sleep. That’s CPAP. And when things get serious-like in respiratory failure-oxygen alone isn’t enough. You need both.
What Happens When You Stop Breathing in Your Sleep?
Obstructive sleep apnea (OSA) happens when the muscles in the back of your throat relax too much. Your tongue and soft tissues collapse, blocking your airway. Each blockage lasts 10 seconds or longer, sometimes over 100 times a night. Your brain wakes you up just enough to gasp for air-but not enough for you to remember it. This cycle repeats, dropping your blood oxygen levels. Your heart races. Your blood pressure spikes. Over time, this wears down your cardiovascular system.
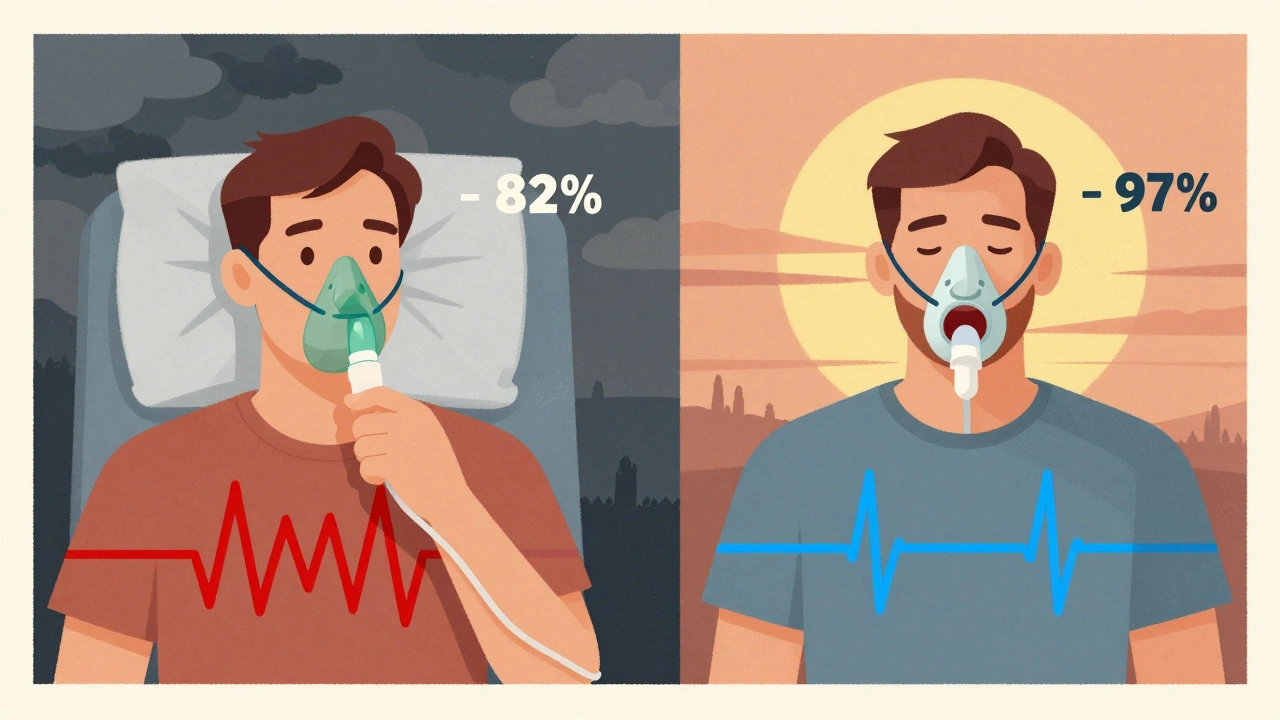
People with severe OSA can have oxygen levels dip below 80% during the night. Normal is 95% or higher. That’s like climbing a mountain without supplemental air. Your body tries to compensate, but it can’t keep up forever. That’s when respiratory failure becomes a real risk-especially if you also have COPD, heart failure, or obesity.
Why Oxygen Therapy Alone Doesn’t Fix Sleep Apnea
You might think: if low oxygen is the problem, just give more oxygen. But that’s like putting a bandage on a broken pipe. Oxygen therapy can raise your blood oxygen levels, but it doesn’t stop the airway from collapsing. You’re still stopping breathing. The root cause remains. In fact, giving oxygen without fixing the obstruction can make things worse. It can mask the problem, delay treatment, and even suppress your natural drive to breathe-especially in people with chronic lung disease.
Studies show that patients with OSA who only get oxygen therapy still have the same number of apnea events. Their blood oxygen may look better on a monitor, but their sleep is still shattered. Their heart is still working overtime. They still wake up exhausted. Oxygen helps symptoms, but it doesn’t treat the disease.
How CPAP Works: The Gold Standard
CPAP-Continuous Positive Airway Pressure-is the most proven treatment for OSA. It works by delivering a steady stream of pressurized air through a mask. That air acts like a splint, holding your throat open so it can’t collapse. No blockage. No pauses. No drops in oxygen. No waking up gasping.
Most machines deliver air between 4 and 20 cm H₂O of pressure. That’s not much-less than the pressure you feel when you blow up a balloon. But it’s enough to keep your airway open. For 90% of people who use it correctly, CPAP reduces apnea events to less than 5 per hour. That’s normal.
There are different mask types: nasal pillows (fit under the nose), nasal masks (cover the nose), and full-face masks (cover nose and mouth). About 73% of users prefer nasal masks. The key? Finding one that doesn’t leak. A leaky mask means pressure drops. The machine can’t do its job. And you’ll still wake up.
When CPAP Isn’t Enough: BiPAP and Auto-CPAP
Some people struggle with CPAP because the constant pressure feels like breathing against a wall-especially when exhaling. That’s where BiPAP (bilevel PAP) comes in. It gives higher pressure when you inhale and lower pressure when you exhale. It’s gentler. Often used for people who need higher pressures (over 15 cm H₂O) or those with heart failure or COPD.
Auto-CPAP (APAP) adjusts pressure automatically throughout the night. It senses when your airway starts to collapse and increases pressure just enough to open it. It’s great for people whose needs change-like if you gain weight, sleep on your back, or get a cold. Studies show it works just as well as fixed-pressure CPAP for most users without major health problems.
CPAP vs. Other Treatments: What Actually Works?
There are alternatives. Mandibular advancement devices (MADs) are mouthpieces that push your lower jaw forward. They help mild to moderate OSA. But for severe cases? CPAP cuts apnea events in half more often than MADs-90% vs. 50%. MADs are easier to use, though. About 70% of people stick with them after a year. CPAP? Only about 50%.
Why the drop-off? Mask discomfort, dry mouth, claustrophobia, and noise. But the biggest reason? Poor setup. People get a machine, a mask, and a brochure. No one shows them how to fit it right. No one checks in after the first week. That’s why adherence is so low.
Here’s what works: in-person fitting. A 2022 survey found patients who got hands-on help from a sleep technician had 32% higher adherence after six months. Also, using heated humidification cuts dry mouth complaints by over half. And chin straps? They solve mouth leaks for nearly half of users.
CPAP and Respiratory Failure: The Life-Saving Link
Respiratory failure doesn’t always mean you’re not breathing at all. Sometimes, it means you’re breathing, but not well enough. Your body can’t get rid of carbon dioxide. Your blood gets too acidic. That’s hypercapnic respiratory failure-common in people with COPD, obesity, or neuromuscular diseases.
That’s where non-invasive ventilation (NIV) comes in. NIV uses a machine similar to CPAP but with more power. It pushes air in and helps pull air out. It’s not just for sleep. It’s used in hospitals for acute attacks. Studies show NIV reduces the need for intubation by 20-30% in COPD flare-ups. If you’re in respiratory failure, CPAP alone won’t cut it. You need NIV-often BiPAP.
Timing matters. If your blood pH doesn’t improve within 1-4 hours of starting NIV, your risk of death goes up. That’s why doctors monitor you closely. This isn’t a home device for long-term use-it’s a rescue tool. But for people with chronic respiratory failure and sleep apnea, NIV can be used nightly at home.
Why Some People Still Fail CPAP
Not everyone who gets CPAP improves. Why? Sometimes, it’s not OSA at all. About 28% of people who don’t respond to CPAP actually have central sleep apnea (CSA)-where the brain doesn’t send the signal to breathe. CPAP doesn’t fix that. You need something else: ASV (adaptive servo-ventilation). But ASV is risky for people with severe heart failure. The SERVE-HF trial showed it increased death rates in that group.
Another reason? Undiagnosed heart disease. The SAVE trial found CPAP didn’t lower heart attack or stroke risk in people with existing heart disease who weren’t sleepy. That doesn’t mean CPAP doesn’t work. It means if you’re not sleepy, the benefits might be limited. Treatment needs to be personalized.

Real People, Real Results
On forums like MyApnea.org, 68% of users say they felt more alert within two weeks of starting CPAP. Others say they stopped snoring so loudly their partner started sleeping in the same bed again. One man in Melbourne, 58, went from needing three naps a day to running 5Ks. His AHI dropped from 42 to 3.
But the complaints are real too. Travel is hard. Masks get lost. Machines break. One Reddit user said he stopped using his CPAP for six months because the hose kept tangling. He started again after switching to a shorter, lighter tube. Another said heated humidification saved her from waking up with a dry throat every morning.
And now, new tech helps. Most modern CPAP machines track your usage. Your doctor can see if you used it 5 hours last night, or if you’re leaking air. Telemonitoring has boosted adherence from 50% to 70% in trials. No more guessing. No more missed appointments.
What’s Next? The Future of Sleep Apnea Treatment
CPAP isn’t perfect. But it’s still the most effective tool we have. In 2023, the FDA approved a new option: an implantable nerve stimulator called Inspire. It’s like a pacemaker for your tongue. It senses when you’re breathing and gently stimulates the nerve to keep your airway open. In trials, 79% of users stuck with it after a year-much higher than CPAP.
But it’s expensive. It requires surgery. And it’s only for people with moderate to severe OSA who can’t use CPAP. For now, CPAP remains the first choice. Especially for people with respiratory failure.
What’s changing? Doctors are moving away from just counting hours. They’re looking at outcomes: Are you less tired? Is your blood pressure down? Is your heart function improving? A 2024 update from the American Academy of Sleep Medicine says adherence goals should be personal. If you’re not sleepy, but your blood pressure improved? That’s a win.
How to Make CPAP Work for You
Here’s what actually helps people stick with it:
- Get fitted by a sleep technician-not just a sales rep. Mask fit matters more than brand.
- Use heated humidification. It cuts dry mouth and nosebleeds.
- Start slow. Use it for 2 hours the first night. Add 30 minutes each night.
- Use a chin strap if you breathe through your mouth.
- Check for leaks. A little air escaping is normal. A lot? Adjust the strap.
- Ask for a follow-up at 72 hours and 30 days. Most clinics don’t offer this-but they should.
- Don’t give up after a bad week. It takes 2-4 weeks to adjust.
And if you’re using oxygen? Talk to your doctor. Are you on CPAP too? If not, you’re not treating the real problem.
What to Do If CPAP Isn’t Working
First: don’t stop. Talk to your sleep specialist. They can:
- Check your mask fit and pressure settings
- Switch you to BiPAP or APAP
- Test for central sleep apnea
- Look for other causes of fatigue-like anemia or thyroid issues
- Refer you to a specialist in complex sleep disorders
There’s always another option. But CPAP is still the most effective starting point.
Can oxygen therapy treat sleep apnea?
No. Oxygen therapy can raise blood oxygen levels, but it doesn’t prevent the airway from collapsing during sleep. Sleep apnea is caused by physical blockage, not low oxygen. Without CPAP or another device to keep the airway open, breathing pauses continue, sleep stays fragmented, and long-term risks remain.
Is CPAP the only treatment for severe sleep apnea?
No, but it’s the most effective. Mandibular devices help mild to moderate cases. Implantable nerve stimulators like Inspire work for some who can’t tolerate CPAP. Surgery is an option too. But for severe obstructive sleep apnea, CPAP remains the gold standard because it stops apnea events in 90% of compliant users.
Can you use CPAP and oxygen together?
Yes, but only if prescribed. Some people with COPD and sleep apnea need both. A special machine called a BiPAP with oxygen integration delivers pressurized air and supplemental oxygen through the same mask. This is common in home care for complex respiratory patients. Never combine them without a doctor’s guidance.
Why do some people stop using CPAP?
The top reasons are mask discomfort, dry mouth or nose, claustrophobia, and leaks. Many also find it hard to travel with or dislike the noise. Poor setup plays a big role-people who get no in-person help are 32% less likely to stick with it. Starting slowly, using humidification, and getting follow-up care dramatically improve long-term use.
Does CPAP help with respiratory failure?
For chronic respiratory failure caused by sleep apnea, yes. But for acute respiratory failure-like during a COPD flare-up-CPAP alone isn’t enough. You need non-invasive ventilation (NIV), often BiPAP, which helps push air in and pull it out. CPAP only pushes air in. NIV is what’s used in hospitals to avoid intubation.
How do I know if my CPAP is working?
Look for these signs: you’re less tired during the day, your snoring stopped, your blood pressure improved, and you’re sleeping through the night. Your machine tracks usage and leak rates. If you’re using it over 4 hours a night, 70% of nights, and your apnea-hypopnea index is below 5, it’s working. Talk to your sleep doctor about your data.
Is CPAP covered by insurance?
In the U.S., Medicare and most private insurers cover CPAP if you’re diagnosed with moderate to severe sleep apnea. They usually require proof of use-typically 4+ hours per night on 70% of nights-for continued coverage. Some insurers now require telemonitoring data. Coverage varies by plan, but the device itself is typically covered after deductible.
Can I travel with my CPAP machine?
Yes. Most modern CPAP machines are lightweight and FAA-approved for air travel. Many have battery options for camping or power outages. Travel cases are available, and some models automatically adjust for altitude changes. Always carry a doctor’s note and your prescription. Airlines allow CPAP as a medical device, not counted as carry-on luggage.

Aileen Ferris
December 10, 2025 AT 18:55Jack Appleby
December 11, 2025 AT 02:36Kaitlynn nail
December 11, 2025 AT 19:46Michelle Edwards
December 12, 2025 AT 20:02Frank Nouwens
December 14, 2025 AT 19:23Nikki Smellie
December 16, 2025 AT 09:39Sarah Clifford
December 16, 2025 AT 15:16Ben Greening
December 18, 2025 AT 11:37Rebecca Dong
December 19, 2025 AT 21:33