Salt Sensitivity – What It Means for Your Blood Pressure
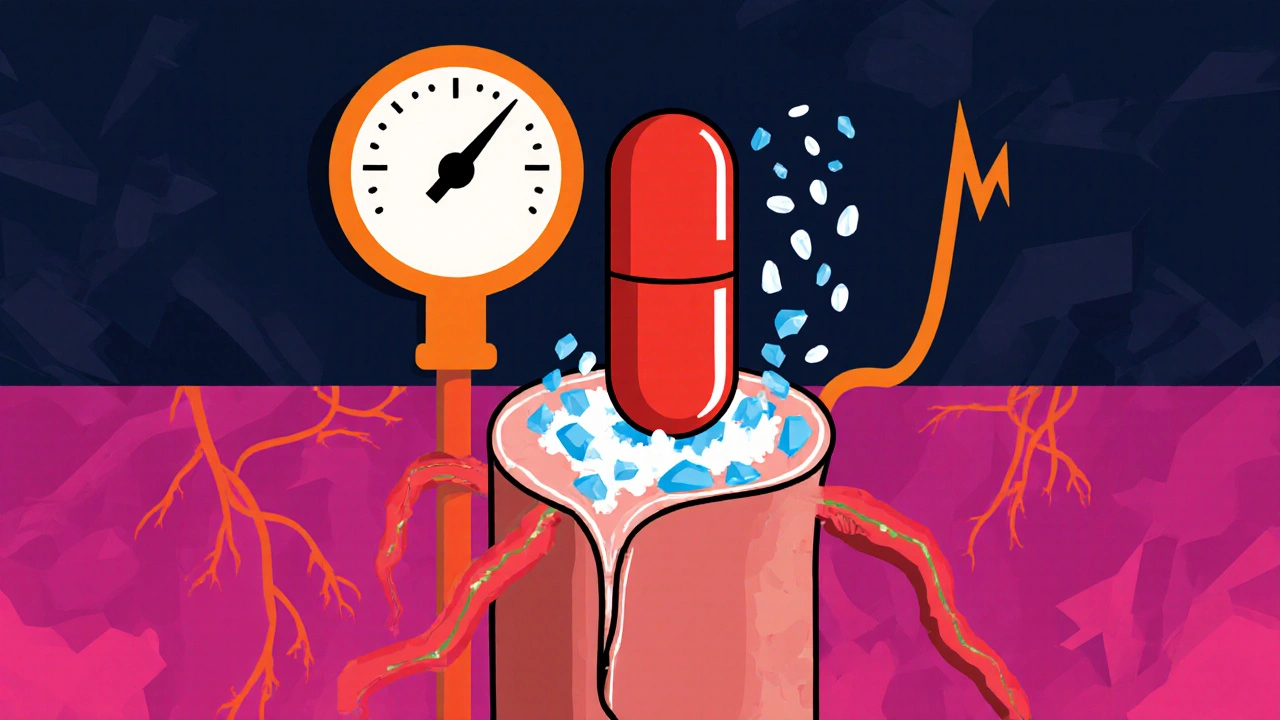
When you hear the term salt sensitivity, you might picture a simple taste preference, but medically it’s a whole different story. Salt sensitivity, the tendency of an individual’s blood pressure to spike after consuming sodium. Also known as sodium‑sensitivity, it affects how the kidneys, blood vessels, and hormonal systems respond to salt. People who are salt‑sensitive often see larger swings in blood pressure after a salty meal, which can increase the risk of heart‑related problems over time. Understanding this trait helps you decide whether cutting back on sodium will actually lower your numbers or if other factors are at play.
One of the clearest connections is between salt sensitivity and hypertension, a chronic condition where blood pressure stays elevated. Hypertension is both a cause and a consequence of salt sensitivity, creating a feedback loop that can damage arteries and the heart. In practical terms, if you know you react strongly to salt, monitoring your blood pressure after meals can give you instant feedback on how your body handles sodium.
But salt isn’t the only player; the amount you eat matters a lot. Dietary sodium, the total salt you ingest through food and drinks directly fuels the salt‑sensitivity response. Processed foods, fast‑food meals, and even some sauces can add up to well over the recommended 2,300 mg per day. When you trim those sources, many salt‑sensitive individuals notice a steady drop in both systolic and diastolic pressures within weeks.
The body’s hormonal control system also plays a crucial role. The renin‑angiotensin system, a network of hormones that regulate blood volume and vessel tone reacts to sodium levels. In salt‑sensitive people, this system often over‑reacts, causing blood vessels to constrict and the kidneys to retain fluid, both of which raise pressure. Medications that block this system, such as ARBs or ACE inhibitors, can blunt the impact of sodium and are a common prescription for those with high salt sensitivity.
Beyond the kidneys and hormones, overall cardiovascular health is at stake. Chronic exposure to high sodium in a salt‑sensitive individual can accelerate atherosclerosis, increase arterial stiffness, and even impair heart‑muscle function. That’s why clinicians look for a combination of blood‑pressure trends, lab tests, and sometimes a salt‑challenge test to decide on treatment pathways. The good news is that lifestyle tweaks—cutting back on processed foods, staying hydrated, and exercising—often provide measurable benefits without the need for medication.
Below you’ll find a curated set of articles that break down these concepts further. Whether you’re looking for drug comparisons, dietary tips, or the science behind how sodium interacts with your body’s systems, the collection provides clear, actionable information to help you manage salt sensitivity effectively.
Amiloride for Salt Sensitivity: How It Can Help Manage High Blood Pressure
Explore how amiloride works, its evidence in salt‑sensitive hypertension, who benefits, dosing tips, side‑effects, and future research in a practical guide.
Read more