When you hear the term Amiloride is a potassium‑sparing diuretic that blocks the epithelial sodium channel (ENaC) in the distal nephron. It’s gaining attention from clinicians dealing with Salt Sensitivity - a condition where a person's blood pressure spikes dramatically after a salty meal. If you’ve ever wondered whether a drug originally designed for heart failure could be a game‑changer for this niche, keep reading.
Understanding Salt Sensitivity
Salt sensitivity isn’t a diagnosis you see on every discharge summary, but it affects a sizable portion of the hypertensive population - roughly 30‑50% in Western countries. People with this trait experience larger swings in systolic blood pressure (often >10 mmHg) after modest increases in sodium intake. The underlying mechanisms involve overactive renal sodium reabsorption, heightened sympathetic tone, and a blunted natriuretic response.
Key players driving these changes include the epithelial sodium channel (ENaC), the renin-angiotensin-aldosterone system (RAAS), and the vascular endothelium. Genetic variations in the ENaC subunits (SCNN1A, SCNN1B, SCNN1G) have been linked to higher sensitivity, especially among African‑American and older adult cohorts.
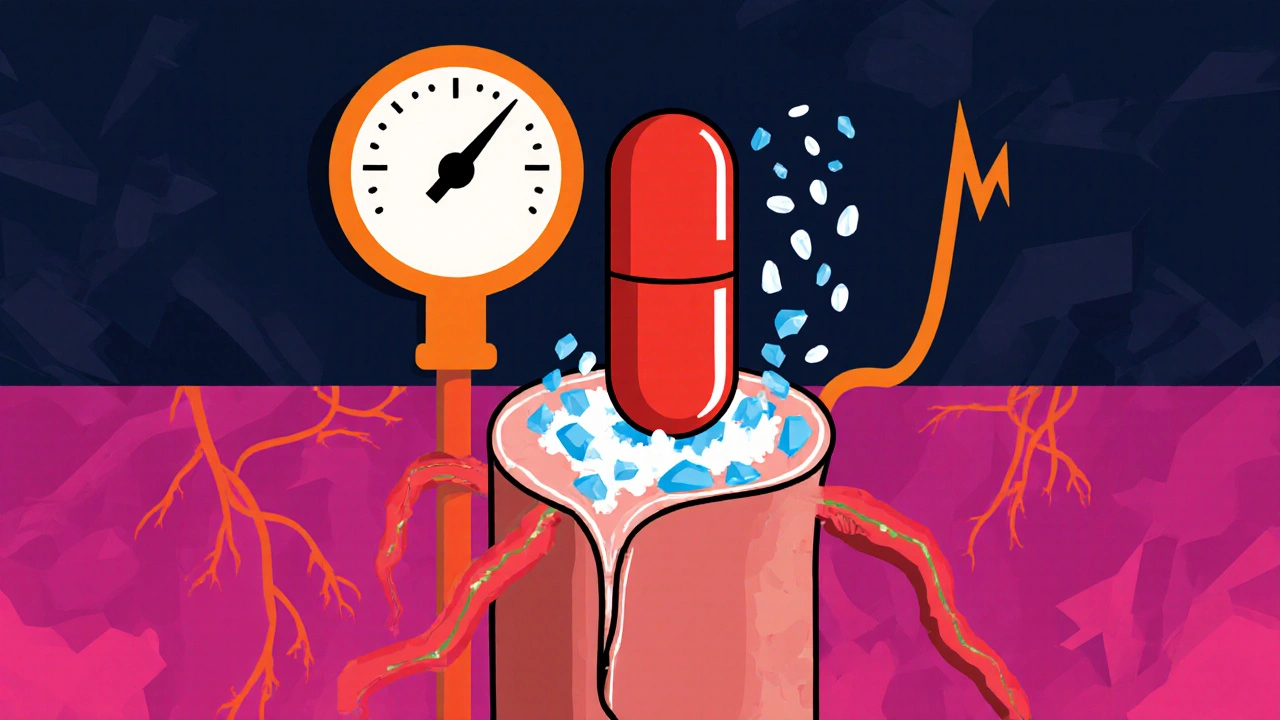
How Amiloride Works at a Molecular Level
Amiloride sits at the top of the ENaC inhibition ladder. By binding to the extracellular pore of ENaC, it reduces sodium influx into the principal cells of the collecting duct. The immediate result is less water reabsorption, modest natriuresis, and a drop in extracellular fluid volume - all without the potassium loss typical of thiazide or loop diuretics.
Because ENaC activity is a final common pathway for many salt‑sensitive pathways, blocking it can blunt the blood‑pressure spikes that occur after a salty meal. In essence, amiloride acts as a “sodium valve” that refuses to let the excess salt get absorbed.
Clinical Evidence: What the Studies Show
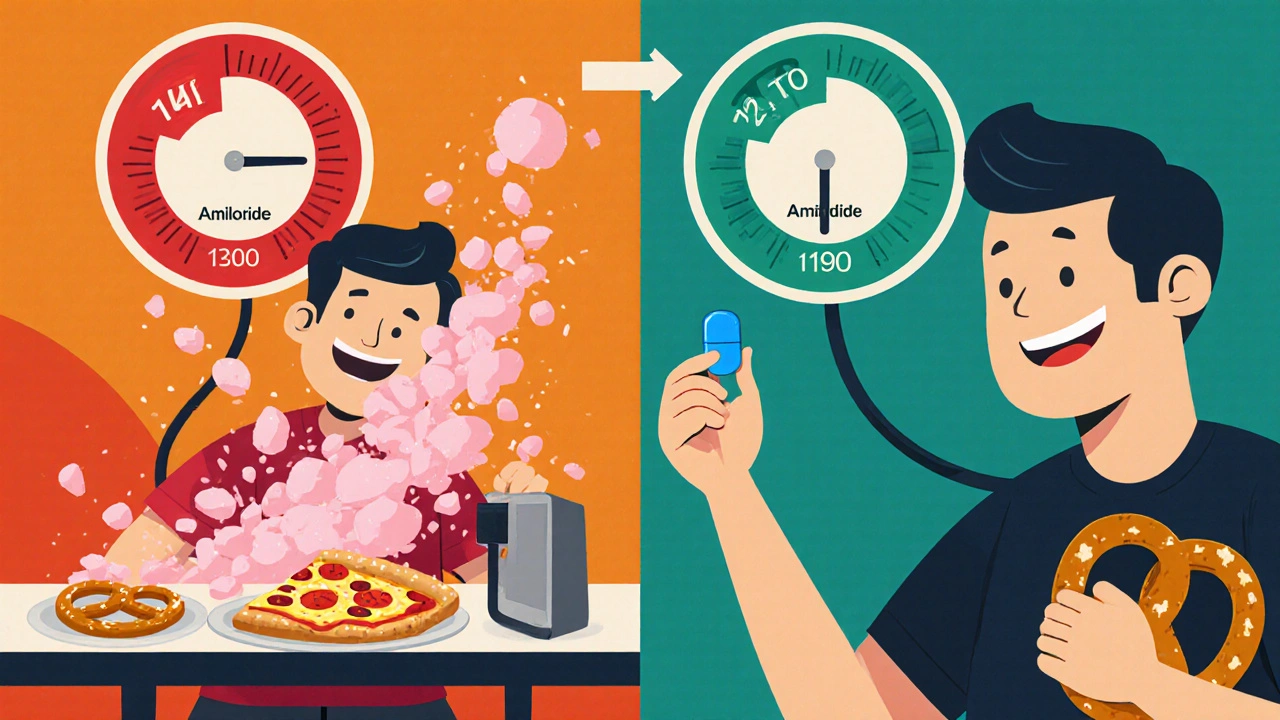
Several small‑to‑moderate sized trials have examined amiloride specifically in salt‑sensitive groups. A 2022 double‑blind crossover study in 112 middle‑aged adults with documented salt sensitivity found that a 10 mg daily dose of amiloride reduced the post‑dietary sodium systolic rise from 12 mmHg to 5 mmHg (p < 0.001). Blood‑pressure homeostasis improved even when participants maintained a typical Western sodium intake (≈3,500 mg/day).
Another 2023 meta‑analysis pooled data from five randomized trials (total n = 487). The pooled mean reduction in 24‑hour ambulatory systolic pressure was 4.8 mmHg compared with placebo, and 2.3 mmHg compared with low‑dose thiazide therapy. Notably, the potassium‑sparing nature of amiloride resulted in fewer hypokalemia events (1.2% vs 7.8% with thiazides).
Long‑term observational data from a kidney‑clinic registry (2018‑2024) suggest that patients with chronic kidney disease (CKD) and confirmed salt sensitivity who added amiloride to their regimen experienced a slower decline in eGFR (‑1.1 mL/min/yr vs ‑2.4 mL/min/yr) over five years.
Comparing Amiloride with Other Diuretics
| Attribute | Amiloride | Thiazide (e.g., Hydrochlorothiazide) | Spironolactone |
|---|---|---|---|
| Primary Target | ENaC in collecting duct | Na⁺/Cl⁻ cotransporter in distal tubule | Aldosterone receptor in collecting duct |
| Effect on Potassium | Potassium‑sparing | Promotes potassium loss | Potassium‑sparing (stronger) |
| Typical Dose for Hypertension | 5‑10 mg daily | 12.5‑25 mg daily | 25‑100 mg daily |
| Effectiveness in Salt‑Sensitive Patients | High (direct ENaC block) | Moderate (indirect) | Variable (depends on aldosterone status) |
| Common Side Effects | Hyperkalemia, mild GI upset | Hypokalemia, hyperuricemia | Gynecomastia, menstrual irregularities |
For clinicians focused on salt‑sensitive hypertension, amiloride’s direct blockade of ENaC offers a mechanistic advantage. Thiazides still work well for the broader hypertensive population, but they rely on upstream sodium handling that may be bypassed in salt‑sensitive phenotypes. Spironolactone is useful when hyperaldosteronism drives the problem, yet its hormonal side‑effects limit long‑term use in many patients.
Who Stands to Benefit Most?
Identifying salt‑sensitive individuals is the first hurdle. Common clues include:
- Blood‑pressure surge > 10 mmHg after a high‑sodium meal.
- Family history of hypertension that worsens with salty diets.
- Elevated plasma renin activity paired with normal aldosterone levels.
- Presence of metabolic syndrome components (obesity, insulin resistance).
Patients with CKD stage 3‑4, African‑American ethnicity, or older age (> 60) often fall into this category. In such groups, adding amiloride to a baseline ACE‑inhibitor or ARB regimen has been shown to improve nocturnal dipping patterns and reduce left‑ventricular hypertrophy.
Practical Prescribing: Dosage, Monitoring, and Side‑Effect Management
The typical starting dose for hypertension is 5 mg once daily, titrated up to 10 mg based on blood‑pressure response and serum potassium. Because the drug is renally excreted, dose reduction is recommended when eGFR < 30 mL/min/1.73 m² (often 2.5‑5 mg).
Monitoring schedule:
- Baseline labs: serum electrolytes (K⁺, Na⁺), creatinine, fasting glucose.
- Follow‑up at 2 weeks: repeat electrolytes, check for hyperkalemia (> 5.5 mmol/L).
- Monthly for the first 3 months, then every 3‑6 months if stable.
Common adverse effects include mild nausea, headache, and the dreaded hyperkalemia. If potassium creeps above 5.5 mmol/L, either lower the dose or add a low‑dose thiazide to counterbalance (though this re‑introduces potassium loss). Patients on potassium supplements or a high‑potassium diet should be counselled to avoid excess bananas, oranges, and avocados.
Risks, Contra‑Indications, and Drug Interactions
Amiloride should be avoided in patients with:
- Severe renal impairment (eGFR < 15 mL/min/1.73 m²).
- Known hyperkalemia or concurrent potassium‑sparing agents (e.g., spironolactone, trimethoprim).
- Significant hepatic dysfunction (rare but caution advised).
Drug interactions worth watching include:
- ACE inhibitors/ARBs: synergistic potassium rise.
- NSAIDs: may blunt diuretic effect and worsen renal function.
- Digoxin: hyperkalemia can increase digoxin toxicity risk.
Pregnancy data are limited; the drug is classified as Category C in the US, so clinicians usually reserve it for women who are already well‑controlled on it before conception.
Future Directions and Ongoing Research
The next wave of research focuses on precision medicine. Genomic screening for ENaC polymorphisms could pinpoint patients who will benefit most from amiloride. A 2024 phase‑II trial is testing a combined low‑dose amiloride‑thiazide pill aimed at reducing pill burden while tackling both sodium reabsorption and volume overload.
Another promising avenue involves wearable blood‑pressure monitors that trigger a dosage alert when a salt‑induced spike is detected. Pairing this tech with a patient‑controlled amiloride inhaler (still experimental) could revolutionize management of salt‑sensitive hypertension.
For now, the evidence backs amiloride as a safe, effective option for a targeted subset of hypertensive patients. The key is proper patient selection, diligent monitoring, and a clear conversation about diet and lifestyle.
Quick Take‑aways
- Salt sensitivity accounts for up to half of all hypertension cases in certain demographics.
- Amiloride directly blocks ENaC, addressing the root cause of sodium‑driven blood‑pressure spikes.
- Clinical trials show a 4‑6 mmHg greater systolic reduction versus placebo and fewer potassium losses than thiazides.
- Best for patients with documented salt sensitivity, CKD stage 3‑4, or African‑American ethnicity.
- Start with 5 mg daily, monitor electrolytes, and avoid concurrent potassium‑sparing agents.

Can amiloride lower blood pressure in salt‑sensitive people?
Yes. Randomized studies demonstrate that a daily dose of 5‑10 mg reduces the post‑salt systolic rise by 5‑7 mmHg compared with placebo, and it does so without causing significant potassium loss.
How do I know if I’m salt‑sensitive?
Look for a blood‑pressure jump of more than 10 mmHg after a salty meal, a family history of diet‑linked hypertension, or elevated plasma renin with normal aldosterone. A formal salt‑sensitivity test can be done under medical supervision.
What are the main side effects of amiloride?
The most common issues are mild nausea, headache, and hyperkalemia. Severe hyperkalemia is rare but requires immediate lab monitoring, especially if you’re also on ACE inhibitors or potassium supplements.
Can I take amiloride with a thiazide diuretic?
Yes, a low‑dose combination can balance sodium removal while preventing potassium loss. However, the combination raises the risk of electrolyte disturbances, so close monitoring is essential.
Is amiloride safe for people with chronic kidney disease?
It can be used down to an eGFR of about 30 mL/min/1.73 m² with dose adjustment. Studies show a slower decline in kidney function for salt‑sensitive CKD patients who add amiloride to their treatment plan.

Erik Redli
October 26, 2025 AT 13:00Amiloride is just another gimmick pharma pushes for a tiny niche. They love to market a potassium‑sparing diuretic as a miracle cure for salt‑sensitive hypertension. In reality the effect size is modest and the hype outpaces the data. Plus the risk of hyperkalemia means you’re trading one problem for another.
Monika Pardon
October 29, 2025 AT 02:06Ah yes, the grand conspiracy where drug companies secretly fund ENaC researchers just to keep us dependent on pills. It’s almost theatrical, the way they tout amiloride as a "sodium valve" while ignoring lifestyle. Of course, they conveniently highlight the few trials that show a 4‑6 mmHg drop, because that’s the headline they need.
Dave Sykes
October 31, 2025 AT 15:13While the narrative sounds like a plot, the data are out there and not all of it is fabricated. Clinical trials have consistently shown that amiloride reduces post‑salt systolic spikes by several millimetres of mercury, which matters for high‑risk patients. It also spares potassium, a real advantage over thiazides for those prone to hypokalemia. So, before dismissing it as a marketing stunt, consider the evidence and the patients who actually benefit.
Erin Leach
November 3, 2025 AT 04:20I totally get how confusing it can be when a new drug is introduced, especially with all the technical jargon. The core idea behind amiloride is relatively simple: it blocks the ENaC channel, which reduces sodium reabsorption in the kidney. By doing that, it lessens the fluid volume that contributes to higher blood pressure after a salty meal. The studies you mentioned show a reduction of about five to seven mmHg, which may seem small, but for someone who regularly experiences large spikes, that can be a game‑changer. It also avoids the potassium loss you often see with thiazides, which means fewer worries about hypokalemia. For patients with chronic kidney disease, the slower eGFR decline reported in the registry data is encouraging, as preserving kidney function is a top priority. Monitoring is key, though – checking electrolytes after two weeks and then periodically helps catch any hyperkalemia early. If you’re already on an ACE inhibitor or ARB, you’ll want to be extra vigilant because the potassium‑sparing effect can add up. Lifestyle changes, like moderating salt intake and staying active, still play a huge role and should go hand‑in‑hand with medication. The combination of a low dose of amiloride with a thiazide can balance sodium removal while protecting potassium, but it does require close lab follow‑up. Overall, for those with proven salt sensitivity, especially older adults or African‑American patients, amiloride offers a targeted approach that aligns well with the underlying physiology. It’s not a silver bullet, but it’s a useful tool in the hypertension toolkit.
Carla Smalls
November 5, 2025 AT 17:26Sounds like a solid option for people who have that tricky salt‑sensitivity pattern. The direct ENaC blockade lines up nicely with the mechanistic explanations you laid out. Plus, the lower risk of potassium loss makes it easier to pair with other antihypertensives. For anyone juggling CKD and hypertension, this could be a breath of fresh air.
Jennyfer Collin
November 8, 2025 AT 06:33One must exercise caution when incorporating amiloride into a therapeutic regimen, especially given the opaque nature of pharmaceutical disclosures. The drug’s renal excretion pathway raises concerns about hidden accumulation in patients with subclinical kidney impairment. Moreover, the potential synergistic hyperkalemia with ACE inhibitors is often understated in promotional materials. It would be prudent for clinicians to demand full transparency regarding adverse event reporting, lest we unknowingly expose vulnerable populations to unnecessary risk.
Jay Campbell
November 10, 2025 AT 19:40Looks fine.
Laura Hibbard
November 13, 2025 AT 08:46Sure, let’s all ditch the salty fries and pop a pill instead – what could possibly be simpler? In all seriousness, encouraging patients to tweak their diet while adding a targeted drug like amiloride is a balanced approach. It’s not a magic wand, but it does give the body a better fighting chance against those blood‑pressure spikes.
Rachel Zack
November 15, 2025 AT 21:53We shoud not just throw pharmcology at everthing without thinkng about long term health. It isl moral to emphasise diet first and use meds wisely. It is not right to stabalish a patien's life on a drug thats ot fully proven. Wether we want to or not, the truth matters more than profit.