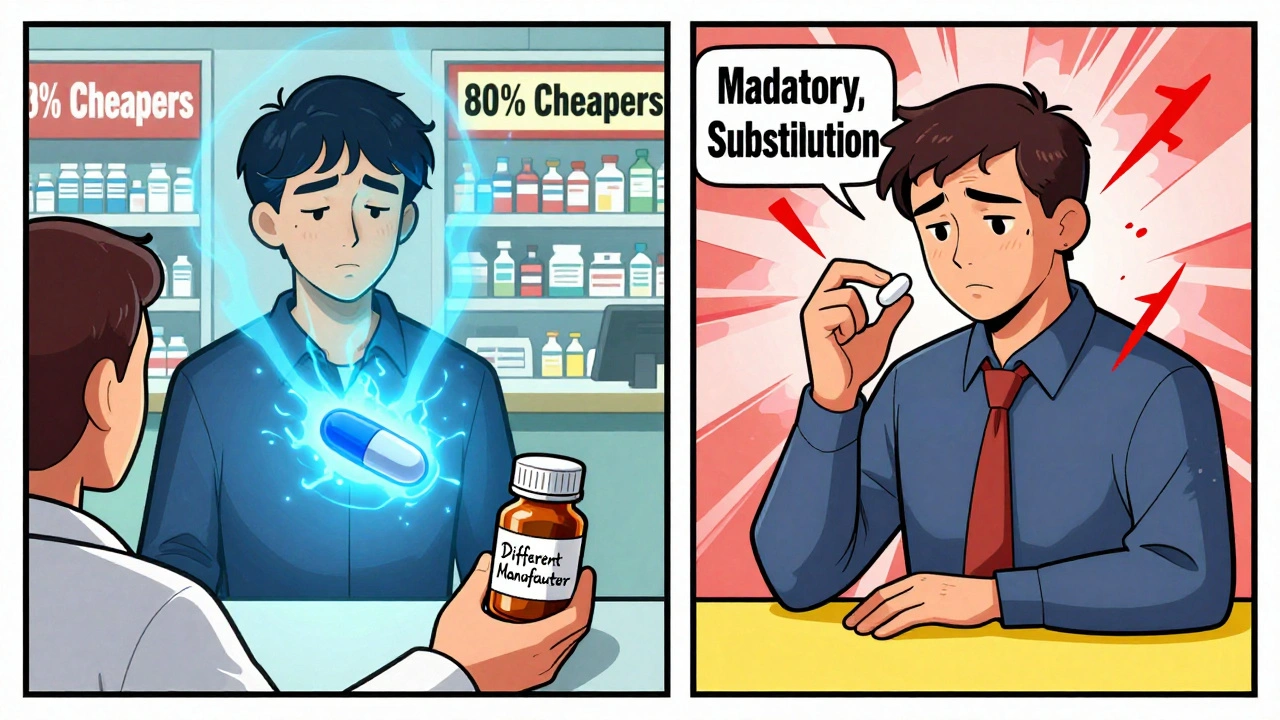
When your pharmacist hands you a pill that looks completely different from what you’ve been taking, it’s normal to feel uneasy. Maybe it’s a smaller white tablet instead of a large blue one. Maybe the name on the bottle is unfamiliar. You’ve just been switched from a brand-name drug to a generic version - and you’re wondering: is this going to work the same?
Why You’re Being Switched
Most of the time, the switch isn’t your doctor’s idea. It’s your pharmacy, your insurance, or the government. Generic drugs cost way less - often 80% to 90% less - than their brand-name cousins. In the U.S., about 90% of all prescriptions are filled with generics. That’s not just a trend; it’s a system designed to save billions. The FDA estimates that generic drugs saved the U.S. healthcare system $370 billion in 2023 alone. Insurance companies push generics because they pay less in copays. Pharmacies get paid more to dispense them. Even governments mandate substitution unless your doctor says "dispense as written." In places like Massachusetts, pharmacists are legally required to substitute generics unless the prescriber blocks it. In Australia, the Pharmaceutical Benefits Scheme (PBS) encourages switching too. The goal is simple: keep people on their meds by making them affordable. But affordability doesn’t always mean ease.Are Generics Really the Same?
The short answer: yes, they are. The FDA requires that generic drugs have the same active ingredient, strength, dosage form, and route of administration as the brand. They must also be bioequivalent - meaning they deliver the same amount of medicine into your bloodstream at the same speed. The acceptable range? 80% to 125% of the brand’s performance. That’s not a loophole; it’s a scientifically accepted margin of error. But here’s what you won’t see on the label: the inactive ingredients. These are the fillers, dyes, preservatives, and coatings. They don’t treat your condition, but they can affect how the pill feels in your mouth, how quickly it dissolves, or whether your body reacts to it. For most people, this makes zero difference. But for a small group - especially those on drugs with a narrow therapeutic index - even tiny changes can matter.When Switching Can Cause Problems
Not all medications are created equal when it comes to switching. Some drugs are extremely sensitive to small changes in blood levels. If your dose drops just a little, your condition might flare up. If it rises too high, you could have side effects. The biggest red flags are:- Anti-seizure medications - Studies show some patients experience more seizures after switching from brand to generic levetiracetam or phenytoin. One 2021 study found 18% of epilepsy patients reported increased seizure frequency after a generic switch.
- Thyroid meds - Levothyroxine (Synthroid) is a classic example. Even slight differences in absorption can throw off TSH levels. Many patients report feeling fatigued, gaining weight, or getting cold after switching to a generic version.
- Blood thinners - Warfarin requires precise dosing. A small change in how your body absorbs the drug can increase bleeding risk or cause clots.
- Immunosuppressants - Drugs like cyclosporine or tacrolimus used after organ transplants must be tightly controlled. Switching has been linked to rejection episodes in rare cases.
What You Might Notice After the Switch
Even if the drug works perfectly, your body might react to the change. Here’s what’s common:- Appearance shock - Your pill changed color, shape, or size. You might think it’s a different drug. Pharmacies often switch manufacturers every few months, so your pill might look different every refill.
- Side effects - You might get a new headache, nausea, or dizziness. It’s not always the active ingredient. Sometimes it’s a dye or filler you’ve never had before.
- Confusion - If you take multiple pills, a change in appearance can make you doubt whether you took your dose. This can lead to missed doses or double dosing.
- Psychological doubt - If you’ve been on a brand-name drug for years, your brain associates that pill with feeling better. A new-looking pill can trigger anxiety, even if it’s chemically identical.
How to Protect Yourself
You don’t have to accept a switch blindly. Here’s how to take control:- Ask your doctor - If you’re on a high-risk medication (thyroid, seizure, blood thinner), ask if you should stay on brand. Say: "I’ve been stable on this. Is switching safe for me?"
- Check the label - Look at the manufacturer name on the bottle. If it changes often, you’re being switched between generics. Keep a note of which one works best for you.
- Monitor your symptoms - Keep a simple log: date, medication, how you feel. If you notice changes in energy, mood, heart rate, or seizure frequency, write it down.
- Don’t panic if you feel off - It could be the switch. Talk to your doctor before stopping. Sometimes it takes a few weeks for your body to adjust.
- Request "dispense as written" - If your doctor agrees, ask them to write this on the prescription. That blocks automatic substitution.
The Cost vs. Risk Trade-Off
Let’s be real: generics save money. The 2019 Association for Accessible Medicines found that patients were 266% more likely to abandon brand-name drugs because of cost. Many people skip doses, split pills, or stop entirely because they can’t afford them. That’s dangerous. A pill you don’t take doesn’t help - no matter how expensive it is. But here’s the paradox: switching can sometimes cost more in the long run. If you end up in the ER because your seizure returned, or your TSH went haywire, the hospital bill could far outweigh the $10 you saved on your prescription. That’s why experts say: don’t switch blindly. Switch smartly.What Experts Say
The FDA says: "There is really no hard proof that generic medications are any less effective or safe than the originals." That’s true for most people, most of the time. But the same agency also acknowledges that some drugs need extra caution. The American Academy of Neurology, the American Thyroid Association, and the American Heart Association all recommend individualized decisions for high-risk drugs. One expert put it simply: "Generic drugs are not always better - but they’re often good enough. Unless they’re not." Harvard Health says: "Taking a generic can save you money and still give you the same results - as long as you pay attention to how you feel."What You Should Do Next
If you’re switching - or thinking about it - here’s your action plan:- For common meds (blood pressure, cholesterol, diabetes): Switching is usually fine. Monitor for a few weeks.
- For high-risk meds (thyroid, seizure, warfarin, transplant drugs): Talk to your doctor before the switch. Ask for a baseline blood test before and after.
- For any drug: Keep your pill bottle. Take a photo of it. If it changes, you’ll know.
- For any change in how you feel: Don’t ignore it. Call your doctor. Don’t wait.
If you’ve been stable for years on a brand-name drug, don’t assume switching is harmless. Ask questions. Track your symptoms. Speak up. Your health isn’t a cost-saving metric - it’s your life.
Are generic drugs as effective as brand-name drugs?
For most people and most medications, yes. The FDA requires generics to have the same active ingredient, strength, and bioequivalence as the brand. Studies show they work just as well in 90% of cases. But for drugs with a narrow therapeutic index - like levothyroxine, warfarin, or anti-seizure meds - even small differences in absorption can matter. If you’ve been stable on a brand, talk to your doctor before switching.
Why do generic pills look different?
Trademark laws prevent generics from looking exactly like the brand-name version. So manufacturers change the color, shape, or size. This isn’t about quality - it’s about legal rules. But it can confuse patients. That’s why some pharmacies put stickers on bottles to warn you when the pill looks different. Keep a photo of your pill, so you know when it’s changed.
Can switching to a generic cause side effects?
Yes - but not because the active ingredient changed. Side effects can come from inactive ingredients like dyes, fillers, or coatings you’ve never taken before. Some people are sensitive to these. If you start feeling new symptoms after a switch - like nausea, dizziness, or fatigue - it could be the new formulation. Don’t ignore it. Contact your doctor.
Should I always choose the cheapest generic?
Not necessarily. Different manufacturers make the same generic drug. One might work better for you than another. If you notice a change in how you feel after switching to a new generic, ask your pharmacist which manufacturer made it. Keep track. You might need to stick with one brand of generic, even if it costs a few dollars more.
How do I stop a switch I don’t want?
Ask your doctor to write "dispense as written" or "no substitution" on your prescription. That tells the pharmacy not to switch you without your doctor’s approval. In some states and countries, this is the only way to block automatic substitution. Don’t assume your doctor knows you want to stay on brand - you have to ask.
Is it safe to switch back and forth between generics?
Frequent switching between different generic manufacturers can increase confusion and risk. Some patients report feeling worse after each switch. If your pill changes every refill, ask your pharmacist why. In some systems, like Saudi Arabia’s, generics are switched every year due to government bidding - and that’s linked to more medication errors. If you’re stable, ask your doctor if you can request a specific generic manufacturer to avoid constant changes.


alaa ismail
December 2, 2025 AT 01:50Just got switched to generic levothyroxine last month. Felt like a zombie for two weeks. Went back to brand after my doc agreed. Worth the extra $15 a month if you’re not sleeping or breathing right.
ruiqing Jane
December 3, 2025 AT 20:56This is exactly why we need better patient education. Most people don’t know they can demand "dispense as written"-and pharmacists rarely tell them. It’s not just about cost, it’s about autonomy. Your body, your rules.
Fern Marder
December 5, 2025 AT 11:29GENERIC SWITCHED MY SEIZURE MEDS. NOW I’M HAVING 3x MORE. MY DOCTOR SAID "IT’S ALL THE SAME." NO IT’S NOT. 🤬
Victoria Graci
December 6, 2025 AT 13:19It’s fascinating how deeply psychological this is. We don’t just take pills-we ritualize them. The shape, the color, the weight in your palm. When that changes, your nervous system doesn’t care about bioequivalence. It cares about familiarity. That’s why some people feel worse even when the science says they shouldn’t. It’s not all in their head-it’s in their body’s memory.
Think of it like switching from your favorite coffee mug to a plain white one. The liquid’s the same, but the ritual breaks. Your brain registers it as loss. And loss, even tiny, triggers stress responses. For someone on a narrow-therapeutic-index drug, that stress can literally alter absorption. The FDA’s 80-125% window? It’s math. But the human body? It’s poetry.
And let’s not pretend this is just about cost. Insurance companies don’t care if you feel like you’re drowning. They care about quarterly reports. Pharmacies don’t care if you’re terrified of your new blue pill. They care about profit margins. We’ve turned medicine into a commodity-and forgotten that healing isn’t transactional.
I’ve seen patients cry because their Synthroid changed from a round white pill to an oval yellow one. Not because it didn’t work. Because they didn’t recognize it. And when you’ve been stable for a decade, that’s a trauma.
So yes, generics are scientifically sound. But science doesn’t live in the body. Culture does. Trauma does. Memory does. Until we acknowledge that, we’re treating symptoms, not people.
Allan maniero
December 7, 2025 AT 06:51Having lived in both the US and the UK, I’ve seen the stark contrast in how generics are handled. In the UK, the NHS has a centralized system where generics are standardized across manufacturers-so you rarely see pill appearance changes. There’s a national formulary, and pharmacists stick to it unless there’s a clinical reason not to. In the US, it’s a free-for-all. Every pharmacy switches based on the cheapest bid that month. You get a different generic every refill. It’s chaos. And it’s not just inconvenient-it’s dangerous for the elderly, the cognitively impaired, and those on critical meds. We need a system that prioritizes stability over savings. A pill shouldn’t be a lottery ticket.
Also, the idea that "90% of prescriptions are generics" sounds impressive until you realize that’s because 90% of people can’t afford the brand. That’s not a win for healthcare-it’s a symptom of a broken system. We should be fighting for affordable brand-name drugs, not normalizing the idea that your medication should be a gamble.
Carolyn Woodard
December 9, 2025 AT 05:26From a pharmacokinetic standpoint, the 80-125% bioequivalence range is statistically valid, but it assumes homogeneity in patient populations, which is a fallacy. Genetic polymorphisms in CYP450 enzymes, gut microbiome variability, and even circadian absorption rhythms can cause divergent responses to identical formulations. The FDA’s framework is built on population averages, not individual physiology. This is why some patients experience clinical deterioration despite bioequivalence-because bioequivalence does not equal clinical equivalence in all contexts. The literature on levothyroxine and cyclosporine is particularly compelling in this regard. We need personalized therapeutic monitoring protocols post-switch, not just passive observation.
Girish Padia
December 9, 2025 AT 10:24People whine about generics like they’re being robbed. Meanwhile, I’m paying $200 for my blood pressure med in India. You want brand? Pay for it. Stop complaining. If you can’t afford it, take the generic. It’s not your body’s fault you’re lazy.
John Webber
December 10, 2025 AT 04:32i had a friend who switched to generic and started having heart palpitations. he went to the er and they said it was anxiety. but he knew. he went back to brand and poof. gone. so yeah. it happens. dont be a dumbass and just accept it.
John Biesecker
December 10, 2025 AT 13:32My grandma switched to generic warfarin and started bruising like a banana. She didn’t say anything for weeks. When we found out, her INR was 5.8. 😣 Doc said "it’s the same" but she’s been on the same brand for 12 years. Now she gets a sticker on her bottle that says "DO NOT SUBSTITUTE." She’s 84. She deserves to not be a lab rat.
❤️
Saravanan Sathyanandha
December 11, 2025 AT 06:15In India, generics are not just common-they’re the backbone of public health. But here’s the nuance: we don’t have the same chaotic switching culture. Once a generic is approved under the National List of Essential Medicines, it’s standardized across suppliers. Pharmacies don’t swap brands monthly. The government ensures batch consistency. So while the cost is low, the stability is high. The American model-driven by pharmacy benefit managers and price bidding-is a different beast. We don’t have the luxury of brand-name drugs for everyone, but we also don’t have the chaos of monthly pill transformations. Maybe the answer isn’t choosing between brand and generic, but between chaos and consistency.
Sheryl Lynn
December 12, 2025 AT 18:00How quaint. You think you’re special because your thyroid feels "off"? Everyone’s thyroid feels off. The real issue is your privilege to even have access to *any* medication. I’ve seen patients in rural Bangladesh who walk 12 miles for a single vial of insulin. You’re crying because your pill changed color? Please. The world doesn’t owe you aesthetic continuity in your pharmaceutical regimen.
Also, your "I feel worse" is not a clinical trial. It’s anecdote. And anecdote is the enemy of evidence-based medicine.
Chelsea Moore
December 13, 2025 AT 01:56I switched to generic levothyroxine and I felt like my soul was being slowly drained. I cried every morning. I gained 20 pounds. My husband said I was "just being dramatic." But I KNEW. I kept a journal. I took photos of my pills. I demanded blood tests. And when my TSH hit 9.1? I went nuclear. I called my senator. I emailed the FDA. I posted on every forum. I got my brand back. And now? I’m alive again. 🙏 This isn’t about money. It’s about dignity. Don’t let them take your stability.
Zoe Bray
December 14, 2025 AT 02:06As a clinical pharmacist with 18 years of experience, I must emphasize that the variability in generic formulations is not a failure of regulation-it is a consequence of market dynamics. The FDA’s bioequivalence standards are appropriate for population-level safety, but they are insufficient for individualized care. When a patient reports a change in clinical status following a generic switch, the appropriate response is not dismissal, but pharmacokinetic re-evaluation, including therapeutic drug monitoring where applicable. Furthermore, the practice of frequent manufacturer substitution-driven by rebate structures and PBM contracts-constitutes an ethical dilemma in patient care. We must advocate for formularies that prioritize therapeutic continuity over marginal cost savings. The patient’s experience is not anecdotal; it is data.