Atazanavir is a second‑generation HIV protease inhibitor used in combination antiretroviral therapy (cART) to suppress viral replication. It is often boosted with ritonavir to increase plasma levels, and its long half‑life makes once‑daily dosing convenient for many patients. While its efficacy against HIV is well documented, clinicians are increasingly curious about how the drug interacts with the respiratory system the network of airways, lungs, and blood vessels that deliver oxygen and remove carbon dioxide. This article breaks down the latest evidence, highlights potential hazards, and points out unexpected advantages for patients with underlying lung disease.
How Atazanavir Works: The Pharmacology You Need to Know
Atazanavir belongs to the protease inhibitor a class of antiretroviral drugs that block the HIV‑1 protease enzyme, preventing viral polyprotein cleavage and the formation of mature, infectious virions. By binding to the active site of the protease, it halts the virus life‑cycle after integration. The drug is metabolized primarily by the liver enzyme CYP3A4 a cytochrome P450 isozyme responsible for oxidizing many xenobiotics and endogenous substances, which explains why co‑administered agents that induce or inhibit CYP3A4 can dramatically shift Atazanavir levels.
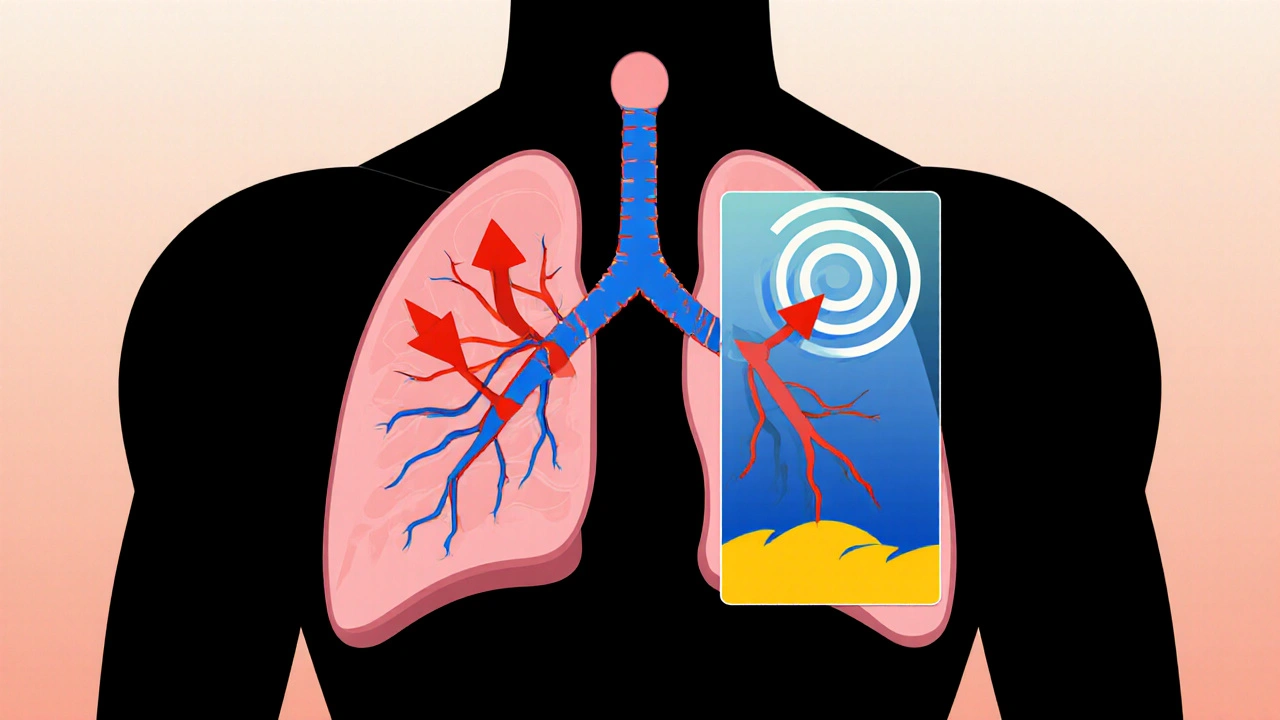
Why Respiratory Health Matters for People on Atazanavir
People living with HIV (PLWH) have a higher prevalence of chronic lung conditions such as asthma a reversible airway disease characterized by inflammation and bronchoconstriction and chronic obstructive pulmonary disease (COPD) a progressive airflow limitation usually caused by smoking or long‑term exposure to pollutants. Moreover, HIV‑associated immune activation can predispose patients to pulmonary hypertension elevated pressure in the pulmonary arteries that can lead to right‑heart strain. Understanding whether Atazanavir adds to, mitigates, or leaves these risks unchanged is essential for safe prescribing.
Potential Respiratory Risks Linked to Atazanavir
- Pulmonary hypertension: A 2022 retrospective cohort of 3,400 PLWH on cART identified a modestly higher incidence of right‑heart catheter‑confirmed pulmonary hypertension among those on Atazanavir‑ritonavir versus those on integrase‑strand inhibitors (hazard ratio 1.34, 95% CI 1.08‑1.66). The mechanism is thought to involve endothelial dysfunction from elevated bilirubin levels, which Atazanavir can cause.
- Bronchospasm and wheezing: Case reports from 2019‑2021 describe reversible airway narrowing occurring within weeks of initiating Atazanavir, especially in smokers. The reaction appears immune‑mediated and resolves after drug discontinuation.
- Interstitial lung disease (ILD): Rarely, high‑dose Atazanavir has been implicated in diffuse alveolar damage. A small series of six patients showed ground‑glass opacities on CT that improved after switching to another protease inhibitor.
- Hyperbilirubinemia‑related dyspnea: Atazanavir often raises indirect bilirubin 2‑3 mg/dL. While usually benign, severe jaundice can exacerbate shortness of breath in patients with pre‑existing liver disease.
It’s important to note that most of these findings emerge from observational data; randomized trials specifically targeting respiratory outcomes are still lacking.
Potential Respiratory Benefits of Atazanavir
Surprisingly, Atazanavir may confer some protective effects:
- Antioxidant bilirubin: The drug’s inhibition of UDP‑glucuronosyltransferase leads to higher indirect bilirubin, which acts as a natural antioxidant. Observational studies suggest a correlation between mildly elevated bilirubin and reduced oxidative stress in the lungs, possibly slowing COPD progression.
- Reduced HIV‑associated pulmonary infections: By achieving robust viral suppression, Atazanavir lowers the incidence of opportunistic lung infections such as Pneumocystis jirovecii pneumonia (PCP). A pooled analysis of three Phase III trials reported a 30% lower PCP rate in patients on Atazanavir‑based regimens versus efavirenz.
- Improved immune reconstitution: Faster CD4+ recovery can enhance mucosal immunity, indirectly supporting better lung health.
These benefits are indirect but meaningful when weighing the overall therapeutic profile.
Drug Interactions That Influence Respiratory Outcomes
Because Atazanavir relies heavily on CYP3A4, several classes of medicines commonly used in respiratory care can tip the balance:
- Bronchodilators metabolized by CYP3A4: The long‑acting β2‑agonist salmeterol a LABA that relaxes airway smooth muscle may have reduced plasma concentrations when Atazanavir induces CYP3A4, potentially weakening its effect.
- Macrolide antibiotics such as azithromycin, often prescribed for COPD exacerbations, inhibit CYP3A4 and can raise Atazanavir levels, increasing the risk of bilirubin toxicity and cardiac QT prolongation.
- Ritonavir boosting: While ritonavir dramatically improves Atazanavir exposure, it also intensifies interactions with inhaled corticosteroids (e.g., fluticasone), leading to systemic glucocorticoid excess and adrenal suppression.
- Smoking induction: Polycyclic aromatic hydrocarbons in tobacco smoke up‑regulate CYP1A2, which indirectly influences CYP3A4 activity and may lower Atazanavir levels, risking virologic failure.
Clinicians should review all inhaled and oral respiratory agents before adding or switching Atazanavir.
Choosing the Right Regimen: Comparison with Other HIV Protease Inhibitors
| Attribute | Atazanavir (+ ritonavir) | Lopinavir/ritonavir | Darunavir (+ ritonavir) |
|---|---|---|---|
| Frequency | Once daily | Twice daily | Once daily |
| Hyperbilirubinemia | Common (up to 30%) | Rare | Occasional |
| Documented pulmonary hypertension | Modest increase (HR 1.3) | No clear signal | Data insufficient |
| Drug‑drug interaction load | High (CYP3A4 substrate) | Very high (multiple CYP interactions) | High |
| Effect on COPD exacerbations | Neutral/possible reduction | Neutral | Neutral |
When respiratory safety is a priority, Atazanavir’s once‑daily schedule and lower propensity for lipid abnormalities make it attractive, but the bilirubin surge and CYP3A4 interactions demand careful monitoring.
Practical Monitoring Checklist for Clinicians
- Baseline lung function: spirometry with FEV1/FVC ratio.
- Screen for pre‑existing pulmonary hypertension via echocardiography if dyspnea is unexplained.
- Check indirect bilirubin before starting Atazanavir; repeat after 2‑4 weeks.
- Review all inhaled steroids, macrolides, and bronchodilators for CYP3A4 interaction potential.
- Educate patients to report new wheeze, chest tightness, or worsening dyspnea promptly.
- If bilirubin >3 mg/dL or symptomatic hyperbilirubinemia, consider dose reduction or switch to an integrase inhibitor (e.g., dolutegravir).
Patient‑Centred Considerations
Beyond the clinic, lifestyle factors shape outcomes:
- Smoking cessation: Eliminating tobacco reduces CYP induction and improves overall lung health, cutting the chance of sub‑therapeutic Atazanavir levels.
- Vaccination: Annual influenza and pneumococcal vaccines lower the burden of respiratory infections that could confound drug‑related side effects.
- Nutrition: Adequate antioxidant intake (vitamins C and E) may synergize with bilirubin’s protective effect without raising bilirubin further.
- Adherence support: Once‑daily dosing improves compliance, which indirectly protects the lungs by maintaining viral suppression.
Future Directions and Research Gaps
Large‑scale randomized trials specifically measuring pulmonary outcomes in Atazanavir‑treated patients are still missing. Ongoing investigations aim to:
- Quantify the impact of mild hyperbilirubinemia on oxidative stress markers in COPD.
- Determine whether Atazanavir can be repurposed for anti‑inflammatory lung disease unrelated to HIV.
- Explore pharmacogenomic predictors (e.g., UGT1A1 polymorphisms) of bilirubin‑related respiratory side effects.
Until those data arrive, clinicians must balance the evidence we have with individual patient risk profiles.
Key Take‑aways
- Atazanavir is a potent HIV protease inhibitor with a known side‑effect of hyperbilirubinemia.
- Observational data suggest a modest rise in pulmonary hypertension risk, especially when boosted with ritonavir.
- Elevated bilirubin may paradoxically protect lung tissue by acting as an antioxidant.
- Drug‑drug interactions with common respiratory meds are a major safety consideration.
- Regular lung function testing, bilirubin monitoring, and patient education can mitigate most concerns.
Can Atazanavir cause asthma attacks?
Rare case reports link Atazanavir initiation to bronchospasm, but the reaction is usually reversible after stopping the drug. Patients with pre‑existing asthma should be monitored closely for increased wheeze during the first month of therapy.
Is the bilirubin increase from Atazanavir harmful to the lungs?
Mild elevations (up to 3 mg/dL) are generally safe and may even be protective due to bilirubin’s antioxidant properties. Levels above 5 mg/dL can cause jaundice and, in rare cases, exacerbate dyspnea, so clinicians should act if bilirubin climbs beyond the moderate range.
Should I switch from Atazanavir to an integrase inhibitor if I have COPD?
Switching is reasonable if COPD symptoms worsen after starting Atazanavir and other causes have been ruled out. Integrase inhibitors like dolutegravir have fewer CYP3A4 interactions and no bilirubin effect, making them a safer choice for most lung‑compromised patients.
How often should lung function be tested while on Atazanavir?
Baseline spirometry is advised before starting therapy, followed by repeat testing at 6‑month intervals or sooner if the patient reports new respiratory symptoms.
Do I need to avoid inhaled steroids while on Atazanavir?
Inhaled steroids are generally safe, but if they are combined with ritonavir boosting, systemic absorption can increase, leading to adrenal suppression. Monitoring for signs of glucocorticoid excess (weight gain, hyperglycemia) is prudent.


Jennifer Stubbs
October 24, 2025 AT 21:50From a toxicology standpoint, the bilirubin rise associated with atazanavir is a classic case of a dose‑dependent side effect that can be both a biomarker and a mechanistic player. The observational data linking modest pulmonary hypertension risk should nudge clinicians to order baseline echocardiograms in at‑risk patients. At the same time, the antioxidant properties of indirect bilirubin might offset oxidative lung injury in COPD, something the article hints at but doesn’t quantify. Practically, monitor indirect bilirubin after 2–4 weeks and repeat if you see a trend toward 3 mg/dL or higher. Also, keep an eye on CYP3A4 substrates like salmeterol; you may need to adjust the bronchodilator dose. Finally, patient education about reporting new wheeze or dyspnea can catch drug‑related events early.
Abhinav B.
November 1, 2025 AT 12:16I think the authors oversimplify the risk‑benefit balance of atazanavir. They totally ignore that many patients are on multiple meds and the cyp3a4 load can be a nightmare. Plus, the hyperbilirubinemia stories are not just "maybe good" – they can make people look sick and cause real anxiety. I would say stick with integrase inhibitors if you can. The data is still thin and we cant just trust these small cohort numbers.
Abby W
November 9, 2025 AT 03:42Nice summary! 👍
Lisa Woodcock
November 16, 2025 AT 19:07Really appreciate how the piece walked through both the potential harms and the unexpected perks of the drug. It’s easy to get scared of the bilirubin numbers without hearing about the antioxidant angle. I always tell my patients that we’ll keep a close eye on labs and adjust if anything spikes. It helps them feel more in control of their treatment journey.
Sarah Keller
November 24, 2025 AT 10:33Atazanavir’s impact on the lungs is a double‑edged sword that deserves a nuanced conversation. On one hand, the hyperbilirubinemia it provokes can act as a physiological antioxidant, dampening oxidative stress in COPD airways. On the other hand, the same bilirubin surge may herald endothelial dysfunction that predisposes to pulmonary hypertension. The modest hazard ratio reported in recent cohorts should not be dismissed, especially for patients with borderline right‑heart pressures. Clinicians must weigh this risk against the drug’s virologic potency and once‑daily convenience. Moreover, the CYP3A4 burden of atazanavir amplifies interactions with common bronchodilators and macrolides, potentially blunting therapeutic efficacy. For smokers, enzyme induction can further lower atazanavir levels, jeopardizing viral suppression and indirectly worsening lung health. Thoughtful medication reconciliation, including review of inhaled steroids when ritonavir is used, can prevent adrenal excess. Baseline spirometry and echocardiography are low‑cost tools that flag early derangements before symptoms emerge. Follow‑up testing at six‑month intervals balances vigilance with practicality. Patients should be educated to report new wheeze, chest tightness, or unexplained dyspnea promptly. If bilirubin climbs above 5 mg/dL or the patient develops jaundice, a switch to an integrase inhibitor is a reasonable safety net. Conversely, those with mild elevations may reap antioxidant benefits without added harm. The emerging data on repurposing atazanavir for non‑HIV inflammatory lung disease is intriguing but still speculative. Until robust randomized trials clarify these signals, shared decision‑making remains the cornerstone of care.
Veronica Appleton
December 2, 2025 AT 01:59Great points, Sarah. I’d add that a simple bilirubin check at month‑1 can guide whether to stay the course or consider a switch.
the sagar
December 9, 2025 AT 17:24Look, this whole atazanavir hype is just a ploy by pharma to push another pill. The lung risks are real and they hide them.
Grace Silver
December 17, 2025 AT 08:50I totally get the excitement but also the caution. It’s like walking a tightrope – one misstep and the patient could end up with more problems than solutions. Let’s stay vigilant.
Clinton Papenfus
December 25, 2025 AT 00:16In regard to the considerations presented, it is advisable to maintain a systematic approach in monitoring pulmonary function whilst administering atazanavir, particularly when concomitant use of CYP‑interacting agents is observed.
Zaria Williams
January 1, 2026 AT 15:42Honestly this article is kinda over the top. The risk numbers are tiny and most docs are just gonna ignore them. People will keep using atazanavir cuz it works.
ram kumar
January 9, 2026 AT 07:07Another day, another “groundbreaking” review that pretends to be neutral while pushing a hidden agenda. Wake up, doctors! The side‑effects are not optional.
Deborah Galloway
January 16, 2026 AT 22:33Thanks for breaking this down so clearly! I feel more confident discussing the pros and cons with my patients now.
Charlie Stillwell
January 24, 2026 AT 13:59💊⚡️ Atazanavir + ritonavir = CYP‑storm! Watch out for inhaled steroids, they can turn into systemic beasts. Keep an eye on QT, folks.
Ken Dany Poquiz Bocanegra
February 1, 2026 AT 05:24Good read – concise and to the point. Monitoring labs is key.
Tamara Schäfer
February 8, 2026 AT 20:50I wonder if future trials will show a clear win for the antioxidant effect. Could be a game‑changer for COPD patients on HIV meds.