Fluoroquinolone Tendon Risk Calculator
This tool helps you assess your risk of tendon rupture when taking fluoroquinolone antibiotics. Based on information from FDA, MHRA, and EMA guidelines, it calculates your risk level based on key factors like age, steroid use, and kidney function.
Fluoroquinolones like ciprofloxacin and levofloxacin carry a serious risk of tendon damage, especially for those over 60, on steroids, or with kidney issues. Early identification of risk can prevent life-changing injuries.
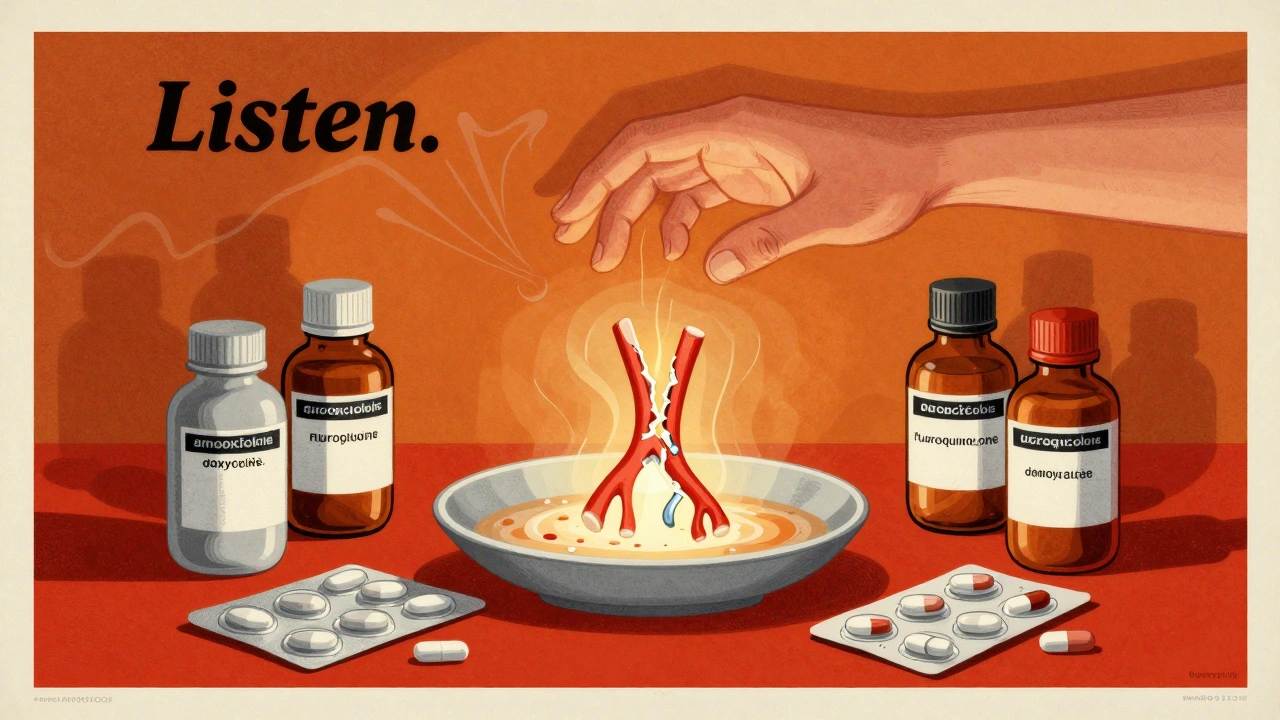
Most people think of antibiotics as simple, safe tools to fight infections. But some of the most commonly prescribed ones - like ciprofloxacin and levofloxacin - carry a hidden danger that can strike without warning: tendon rupture. If you’ve been prescribed a fluoroquinolone antibiotic, especially if you’re over 60, on steroids, or have kidney issues, you need to understand the real risk - not just the fine print, but what it means for your body.
What Are Fluoroquinolones, and Why Are They Still Prescribed?
Fluoroquinolones are a class of powerful antibiotics developed in the 1960s. They work against a wide range of bacteria, which made them popular for treating everything from urinary tract infections to pneumonia. Today, about 25 million fluoroquinolone prescriptions are written every year in the U.S. alone. That’s a lot of people taking them. But here’s the problem: these drugs don’t just kill bacteria. They can also damage your tendons - the tough cords that connect muscle to bone. The Achilles tendon, behind your ankle, is the most vulnerable. Studies show it’s involved in nearly 90% of all fluoroquinolone-related tendon injuries. And it’s not just one tendon - up to half of cases affect both sides. The U.S. Food and Drug Administration (FDA) put a black-box warning on these drugs in 2008. That’s the strongest warning they can give. It means: this can cause serious, even permanent, harm. The UK’s MHRA and Europe’s EMA followed with similar restrictions. Today, doctors are told to avoid fluoroquinolones unless there’s no other option - like for life-threatening infections such as anthrax or complicated kidney infections.Who’s at the Highest Risk?
Not everyone who takes these antibiotics gets tendon damage. But certain people are at dramatically higher risk.- Age 60 and older: Your tendons naturally weaken with age. Combine that with fluoroquinolones, and your risk of rupture jumps. People over 80 have a 20 times higher chance than younger adults.
- Corticosteroid users: If you’re taking prednisone or another steroid - even a short course - your risk of tendon rupture increases by 46 times. This combination is one of the most dangerous in all of medicine.
- People with kidney disease: Fluoroquinolones are cleared by the kidneys. If your kidneys aren’t working well, the drug builds up in your system, increasing toxicity.
- Those with diabetes or organ transplants: These conditions affect tissue repair and immune response, making tendons more fragile under drug stress.
- Previous tendon injury: If you’ve had a tendon problem before, you’re far more likely to have another one.
When Does Tendon Damage Happen?
One of the scariest things about fluoroquinolone-induced tendinopathy is how unpredictable it is. You might think the danger is only while you’re taking the drug. But it’s not that simple.- Most cases start within 6 days of starting the antibiotic.
- 85% of tendon pain or swelling shows up within the first month.
- But symptoms can appear months after you’ve stopped taking the drug. One case was reported 6 months later.
- In some extreme cases, pain began just two hours after the first pill.
How Does This Actually Happen?
It’s not just an allergic reaction. Fluoroquinolones attack your tendons at a cellular level. These drugs interfere with an enzyme called topoisomerase II, which your body uses to repair DNA. That’s fine in bacteria - it kills them. But your own cells, especially in tendons, use the same enzyme. When it’s blocked, your tendon cells start dying off. At the same time, fluoroquinolones trigger the release of harmful chemicals like nitric oxide, which further break down tendon tissue. They also bind to magnesium and calcium - minerals your tendons need to stay strong. The Achilles tendon is especially vulnerable because it’s under constant stress. It’s the strongest tendon in the body, but it’s also the one that bears the most load. When it’s weakened by a drug, even walking or standing can push it over the edge.What Do the Studies Really Say?
You might hear conflicting information. One study says fluoroquinolones are dangerous. Another says they’re fine. What’s going on? Large population studies tell a clear story. A UK analysis of 6.4 million people found fluoroquinolone users had a 4.3 times higher risk of tendinitis and a 2 times higher risk of actual tendon rupture. A Taiwanese study of over 350,000 patients confirmed this - those taking fluoroquinolones had nearly double the rate of tendon disorders. But a 2022 study in Japan looked at 504 people with ruptured Achilles tendons and found no link to fluoroquinolones. Why the difference? The Japanese study used a different method - comparing patients to themselves before and after taking the drug. That approach can miss subtle, long-term risks. Other studies used much larger groups and real-world data, which are more reliable. The FDA, MHRA, and EMA all agree: the risk is real. The few studies that downplay it are outliers. When over a dozen major studies point the same way, you don’t ignore them.What Should You Do If You’re Prescribed One?
If your doctor suggests a fluoroquinolone, ask these questions:- Is there another antibiotic that could work just as well?
- Am I in a high-risk group (age 60+, on steroids, kidney issues)?
- What are the signs of tendon damage I should watch for?
- What should I do if I feel pain in my tendons?
What Happens If Your Tendon Ruptures?
A ruptured tendon isn’t just painful - it’s life-changing. You might hear a pop. Your ankle or shoulder might suddenly feel weak. Walking becomes impossible. Surgery is often needed. Recovery takes months. Physical therapy is grueling. Some people never fully regain their strength. And the damage isn’t always visible on an MRI. In many cases, the tendon is already weakened long before it breaks. That’s why early symptoms - even just mild discomfort - are so important to act on.Are There Alternatives?
Yes. For most common infections - like bladder infections, sinus infections, or bronchitis - there are safer antibiotics:- Amoxicillin
- Doxycycline
- Cephalexin
- Nitrofurantoin (for UTIs)
Final Thoughts
Fluoroquinolones aren’t evil drugs. They save lives in serious infections. But they’re not harmless either. Their risks are real, predictable, and preventable - if you know what to look for. If you’re over 60, on steroids, or have kidney trouble, treat these antibiotics like a loaded gun. Don’t take them unless you absolutely have to. And if you do, watch your tendons like a hawk. Pain isn’t just a side effect - it’s a warning sign. Your body doesn’t always scream before it breaks. Sometimes, it just whispers. Listen.Can fluoroquinolones cause tendon rupture even after I stop taking them?
Yes. While most tendon issues start within the first month of taking fluoroquinolones, symptoms - including rupture - can appear weeks or even months after you’ve finished the course. The drug can linger in tendon tissue and continue causing damage. If you develop sudden pain or swelling in a tendon after stopping the medication, seek medical help immediately.
Which fluoroquinolone has the highest risk of tendon damage?
Levofloxacin is the most commonly linked to tendon problems, followed by ciprofloxacin. Moxifloxacin carries a lower risk, but it’s still present. All fluoroquinolones carry the same black-box warning from the FDA. No one in this class is considered safe for high-risk patients.
Is tendon damage from fluoroquinolones reversible?
Mild tendinitis can improve with rest and stopping the drug. But once a tendon ruptures, it usually requires surgery and long-term rehab. Even then, many people don’t fully regain their strength or mobility. In some cases, chronic pain and weakness last for years. Early intervention is the only way to avoid permanent damage.
Should I avoid fluoroquinolones if I’m active or an athlete?
Yes. Athletes and active individuals are at higher risk because their tendons are under constant stress. Even if you’re young and healthy, the combination of physical strain and fluoroquinolone use increases the chance of sudden rupture. Always ask for an alternative, especially for non-life-threatening infections.
What should I do if I feel tendon pain while on a fluoroquinolone?
Stop taking the medication immediately. Avoid putting weight or strain on the painful area. Contact your doctor right away. Do not wait to see if it gets better. Early action can prevent a full rupture. Your doctor will likely switch you to a safer antibiotic and may recommend imaging or immobilization.


kevin moranga
December 12, 2025 AT 13:46Man, I wish I’d known this before I took cipro for that UTI last year. I was hiking, felt a weird twinge in my Achilles, thought it was just a cramp. Two days later? Full rupture. Surgery. Six months of PT. Now I tell everyone I know: if your doc pushes a fluoroquinolone, ask for something else. They’re not magic bullets - they’re landmines in pill form.
Lara Tobin
December 14, 2025 AT 11:36I’m so glad someone finally said this out loud. My mom took levofloxacin after a sinus infection and couldn’t walk for weeks. She didn’t even know it was the drug until a rheumatologist connected the dots. Please, if you’re reading this and your doctor’s about to prescribe one - speak up. You’re not being difficult. You’re being smart.
Keasha Trawick
December 15, 2025 AT 21:52This isn’t just a side effect - it’s a biochemical betrayal. Fluoroquinolones don’t just inhibit bacterial topoisomerase II - they hijack your mitochondrial DNA repair machinery like a rogue AI in a sci-fi horror flick. Magnesium chelation? Nitric oxide storms? Tendon cells turning into apoptotic confetti? This isn’t medicine - it’s molecular sabotage with a prescription label. And we’re still handing these out like candy at Halloween?
Yatendra S
December 17, 2025 AT 00:18Life is pain 🤕. But the real pain? When your body turns against you because someone thought ‘broad-spectrum’ meant ‘universal solution.’ We chase efficiency in medicine and forget that biology isn’t a spreadsheet. 🌱
Webster Bull
December 17, 2025 AT 10:30stop the drug. no wait. call doc. now. your tendons ain’t gonna fix themselves. been there. done that. dont be the guy who ignored the whisper.
Himmat Singh
December 17, 2025 AT 23:49It is intellectually dishonest to characterize fluoroquinolones as inherently dangerous. The data, while statistically significant in aggregate, reflects confounding variables including age, polypharmacy, and pre-existing connective tissue disorders. To vilify an entire class of antimicrobials based on population-level epidemiology is to misunderstand the nature of medical risk-benefit analysis. The FDA’s black box warning is appropriate, but public discourse has devolved into fearmongering.
Bruno Janssen
December 19, 2025 AT 14:01I’ve been on cipro three times. Two of them, I felt that dull ache in my heel. I ignored it. Now I can’t run. I can barely climb stairs. And the worst part? No one believes me when I say it was the antibiotic. They just say ‘you’re old’ or ‘you overdid it.’ But I was 32. I didn’t overdo anything. They just didn’t care.
Tom Zerkoff
December 20, 2025 AT 13:25Thank you for this meticulously researched and clinically grounded exposition. The epidemiological evidence is unequivocal, and the mechanistic pathways - particularly the chelation of divalent cations and the induction of oxidative stress in tenocytes - are well-documented in peer-reviewed literature. As a healthcare professional, I now explicitly counsel all patients over 50 against fluoroquinolone use unless absolutely necessary, and I document the discussion in writing. Prevention is not just prudent - it is ethically imperative.
Scott Butler
December 21, 2025 AT 17:05Stop the fear-mongering. America’s healthcare system is already collapsing because people won’t take antibiotics when they’re needed. You think we should go back to the 1950s where pneumonia killed people because we were too scared to use the best tools? This isn’t about tendon pain - it’s about cowardice disguised as caution. If you’re too fragile to take a pill, maybe you shouldn’t be hiking.