The skin around your eyes is the thinnest on your entire body-just 0.55 millimeters thick. That’s why even a tiny bit of an allergen can trigger a nasty reaction: redness, swelling, itching, flaking, or even tiny blisters. If you’ve had a recurring eyelid rash that won’t go away, no matter how much you change your makeup or wash your face, you’re not alone. About 74% of eyelid dermatitis cases are caused by allergic contact dermatitis (ACD), according to a 2023 NIH study. And most of the time, the culprit isn’t what you think.
Why Your Eyelids Are So Sensitive
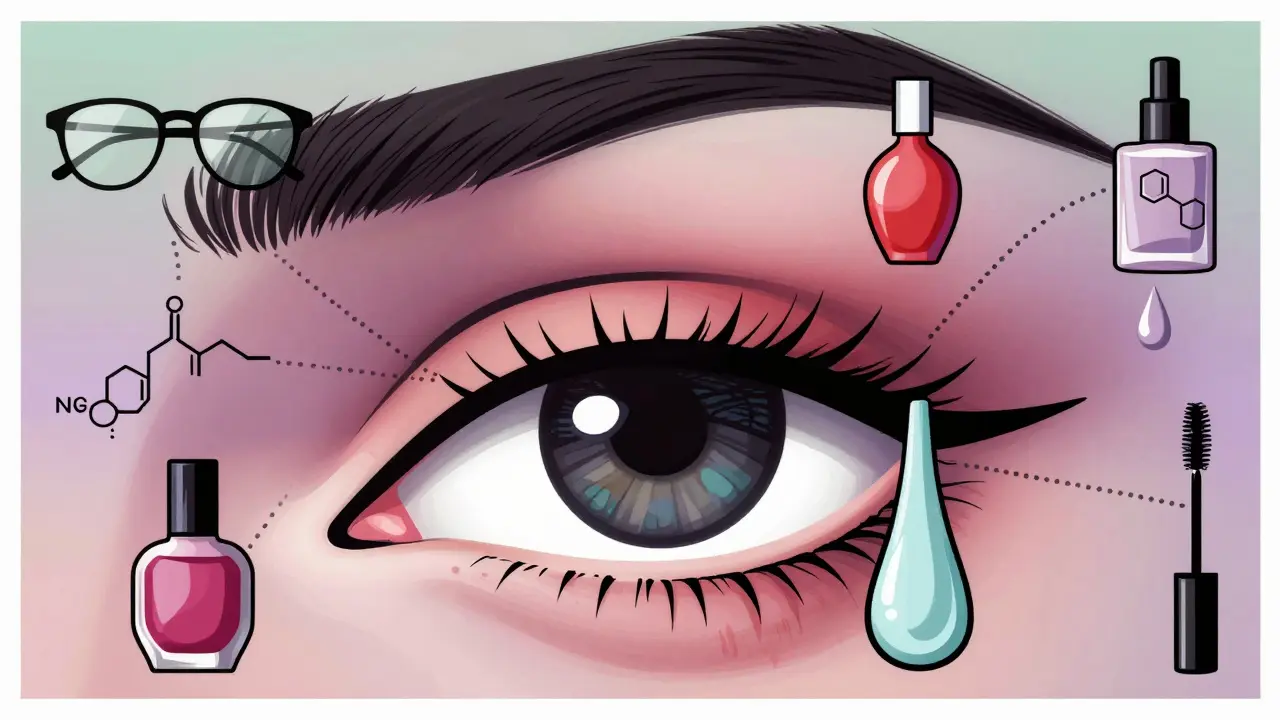
Your eyelids aren’t just delicate-they’re exposed. Every day, you touch them with your hands after applying nail polish, washing your hair, or using hand cream. You rub them when you’re tired. You apply eye creams, mascaras, concealers, and even sunscreen right on top of them. All of that adds up. The skin there doesn’t have much of a protective barrier, and it traps allergens in its natural folds. That’s why even products you’ve used for years can suddenly start causing problems.The Top 6 Allergens You’re Probably Using Right Now
Most people assume their eyelid rash comes from cheap or expired makeup. But research shows something different. In a 2021 study of 215 patients with eyelid dermatitis, the biggest offenders weren’t the big-name brands-they were hidden ingredients:- Nickel (28.7%): Found in cheap jewelry, eyeglass frames, and even some mascara wands. It’s the #1 cause of eyelid allergies.
- Shellac (21.4%): Used in gel nail polishes. If you get your nails done regularly, you’re likely transferring it from your fingers to your eyes.
- Preservatives (18.9%): Parabens, formaldehyde releasers (like DMDM hydantoin), and methylisothiazolinone are in almost every cosmetic product labeled "hypoallergenic."
- Topical antibiotics (15.3%): Neomycin and bacitracin, often found in over-the-counter eye ointments, can trigger reactions in people who don’t even realize they’re using them.
- Fragrances (14.6%): Even "natural" scents like lavender or tea tree oil can cause reactions. The word "fragrance" on a label hides dozens of chemicals.
- Acrylates (12.1%): Used in long-wear, waterproof makeup and false lashes. These are becoming more common as "smudge-proof" products grow in popularity.
What’s surprising? Fragrances and preservatives are usually top triggers in general contact dermatitis-but on the eyelids, nickel and shellac are bigger threats. And here’s the kicker: 42% of cases come from indirect exposure. You didn’t put the product on your eyelids-you touched your nails, then rubbed your eyes.
Why Your Doctor Might Be Missing the Real Cause
Many general practitioners and even some ophthalmologists assume eyelid irritation is from dry eyes, blepharitis, or an infection. They’ll prescribe steroid drops or antibiotic ointments. But if the real problem is an allergen, those treatments won’t help-and might make things worse.Dr. Erin Warshaw from Wake Forest School of Medicine says clinical history alone identifies the right trigger in only 37% of cases. That means more than 6 out of 10 people are guessing. If your rash keeps coming back after you "clean up" your routine, it’s not your fault. You just need better testing.
How Patch Testing Works (And Why It’s Essential)
Patch testing is the gold standard for diagnosing eyelid dermatitis. It’s not a skin prick or a blood test. It’s a 48- to 72-hour slow burn. Small patches with 60-100 common allergens are taped to your back. You don’t shower or sweat during that time. Then, a dermatologist checks for reactions.When done right-with an expanded panel that includes ophthalmic-specific allergens like acrylates and shellac-it’s 89% accurate. The standard TRUE Test panel misses many eyelid triggers. That’s why specialists now recommend adding extra patches for nail products, hair dyes, and preservatives found in eye care items.
One patient, "MakeupLover87," spent three years trying everything before patch testing revealed she was reacting to toluene sulfonamide formaldehyde resin-a common ingredient in gel nail polish. Once she stopped getting her nails done, her eyelids cleared up in 48 hours.

What to Do While Waiting for Test Results
Don’t wait months to feel better. Follow this simple 3-phase plan:- Days 1-3: Stop everything. No makeup, no eye creams, no scented lotions near your eyes. Use only plain petroleum jelly (like Vaseline) to moisturize. Avoid touching your eyes with your hands.
- Days 4-14: Cool compresses and patience. Apply a clean, cool, damp cloth to your eyelids for 5-10 minutes, twice a day. This reduces swelling and itching. Don’t use steroid creams unless prescribed by a dermatologist-high-potency steroids can cause permanent thinning of the eyelid skin in as few as 7-10 uses.
- Day 15+: Targeted avoidance. Once you know your allergens, you can shop smart. Use the Contact Allergen Replacement Database (CARD), updated monthly by the University of Louisville. It lists over 12,800 verified safe products across 188 categories, from mascara to moisturizers.
Reading Labels Like a Pro
Cosmetic ingredients are listed in INCI (International Nomenclature of Cosmetic Ingredients). That means "fragrance" might hide 50 chemicals. "Methylisothiazolinone" is a preservative. "Toluene sulfonamide formaldehyde resin" is a nail polish ingredient. You don’t need to memorize them all-but you can use apps like Preservative Finder, downloaded over 147,000 times by 2023, to scan product barcodes and flag risky ingredients.Even "clean beauty" products aren’t safe. A 2023 JAMA Dermatology study found 33% of "natural" eye products contained Compositae plants (like chamomile or daisies), which are common allergens for sensitive skin. Just because it’s organic doesn’t mean it won’t irritate you.
Why This Isn’t Just a Skin Problem
Eyelid dermatitis often signals a bigger pattern. About 63% of people with eyelid allergies also react to the same allergens on their hands, neck, or face. That’s why dermatologists look at your whole body-not just your eyes. If you’re allergic to nickel in your earrings, you might also react to it in your phone case or belt buckle.And here’s something most people don’t know: eyelid dermatitis rarely leads to skin cancer. It’s not a sign of something dangerous-it’s a sign of something you’re touching too often.

New Treatments and What’s Coming
In December 2022, the FDA approved Eysuvis (0.25% loteprednol etabonate), the first steroid ointment specifically designed for eyelid use. Clinical trials showed 89% of patients saw symptom relief in 14 days without eye pressure or cataract risks. It’s a game-changer for people who can’t tolerate traditional steroids.On the horizon: AI tools like DermAI Contact, launched in beta in 2023. It analyzes your symptoms, product history, and rash pattern to predict likely allergens before you even get to the dermatologist. It’s 76% accurate-helping cut down testing time and guesswork.
But new products bring new risks. Magnetic eyelashes, now trending, contain tiny nickel alloys. They’re convenient-but they’re also a rising cause of eyelid reactions. Experts warn that without better labeling and awareness, these innovations could undo progress.
What Works-and What Doesn’t
Here’s what patients report after following a targeted plan:
- 52% saw full improvement in 1-2 weeks after avoiding their allergens.
- 29% needed 3-6 weeks because they missed one hidden source (like shampoo runoff or hand cream).
- 19% needed extra treatment because inflammation had become chronic.
- Those who got detailed ingredient lists from patch testing had a 68% success rate.
- Those who just heard "avoid makeup" had only a 32% success rate.
Generic advice doesn’t work. You need to know exactly what to avoid.
Final Takeaway
Eyelid dermatitis isn’t just a nuisance. It’s a signal. Your skin is telling you something about what you’re exposing yourself to. It’s not about being allergic to makeup-it’s about being allergic to one specific chemical hiding in it. The good news? Once you find it, you can make your eyelids feel normal again. And you don’t need to give up makeup forever. You just need to know what’s safe.Can eyelid dermatitis go away on its own?
Sometimes, if you stop using the trigger product, symptoms can improve in a few days. But if you keep using it-even occasionally-the rash will come back. Without identifying the exact allergen, you’re just guessing. That’s why patch testing is the only way to be sure it’s truly gone for good.
Is it safe to use hydrocortisone cream on my eyelids?
Only under a dermatologist’s guidance. Over-the-counter hydrocortisone (1%) is low potency and may be safe for short-term use on the eyelids. But stronger steroids-even those labeled "for sensitive skin"-can cause skin thinning, stretch marks, or even glaucoma if used too long. Never apply steroid creams to your eyelids without knowing the exact diagnosis.
Why does my eyelid rash flare up after I wash my hair?
Shampoos, conditioners, and hair dyes often contain allergens like fragrances, preservatives, or paraphenylenediamine (PPD). When you rinse your hair, these chemicals can run down your face and settle on your eyelids. Even if you don’t get product in your eyes, the runoff is enough to trigger a reaction. Try rinsing your face before washing your hair, or wear a shower cap.
Can I still wear mascara if I have eyelid dermatitis?
Yes-but only after you know what you’re allergic to. Many mascaras contain nickel, acrylates, or preservatives like methylisothiazolinone. Use the CARD database to find verified safe brands. Look for products labeled "oculoplastic tested" or "ophthalmologist approved." And always patch test a new product on your inner arm for 48 hours before using it near your eyes.
Do I need to throw away all my makeup?
Not necessarily. If you’re allergic to a specific ingredient, you can keep products that don’t contain it. But if you’re unsure, it’s safer to replace anything you applied near your eyes during the flare-up. Bacteria and allergens can linger in brushes and tubes. Start fresh with one new product at a time, and track what triggers a reaction.
Is eyelid dermatitis contagious?
No. It’s not caused by bacteria, viruses, or fungi. You can’t catch it from someone else. It’s an immune reaction to a chemical you’ve come into contact with. That means your partner can use the same lipstick or eye cream without risk-unless they’re also allergic to the same ingredient.
How long does patch testing take?
The process takes about 5 days. Patches are applied on Day 1, left on for 48 hours, then removed. You return on Day 4 for the first reading, and Day 5 or 6 for a final check. Some reactions appear slowly, so the final reading is critical. Results are usually available within a week, and your dermatologist will give you a list of safe and unsafe ingredients.

jenny guachamboza
December 22, 2025 AT 13:24Sam Black
December 23, 2025 AT 22:52Tony Du bled
December 25, 2025 AT 09:06Kathryn Weymouth
December 27, 2025 AT 03:48Nader Bsyouni
December 27, 2025 AT 08:16Julie Chavassieux
December 28, 2025 AT 01:43Herman Rousseau
December 29, 2025 AT 07:40Ajay Brahmandam
December 29, 2025 AT 21:15Cara Hritz
December 30, 2025 AT 18:15Jamison Kissh
January 1, 2026 AT 16:09Aliyu Sani
January 1, 2026 AT 18:16Gabriella da Silva Mendes
January 3, 2026 AT 09:35Kiranjit Kaur
January 3, 2026 AT 15:36Art Van Gelder
January 4, 2026 AT 21:55