Migraine with Aura Stroke Risk Calculator
If you get migraines with aura and are thinking about birth control, you’re not alone. But you’re also facing a decision that could affect your long-term health in ways most people don’t talk about. The question isn’t just migraine with aura and birth control - it’s whether that combination could raise your chance of having a stroke. And the answer isn’t as simple as ‘yes’ or ‘no.’
What Exactly Is Migraine with Aura?
Migraine with aura isn’t just a bad headache. It’s a neurological event. Before the pain hits, you might see flashing lights, blind spots, or zigzag lines. Some people feel tingling in their hands or face, or even have trouble speaking. These symptoms last 5 to 60 minutes and are called aura. They’re not side effects - they’re actual changes in brain activity.
It’s important to know what counts as aura. Nausea, sensitivity to light, or feeling tired? Those are warning signs, but not aura. Only focal neurological symptoms - things that affect your vision, speech, or sensation - qualify. If you’ve ever had a moment where you couldn’t find the right word or your vision went blurry for 20 minutes, that’s likely aura. And if you’ve had it even once, that changes your birth control options.
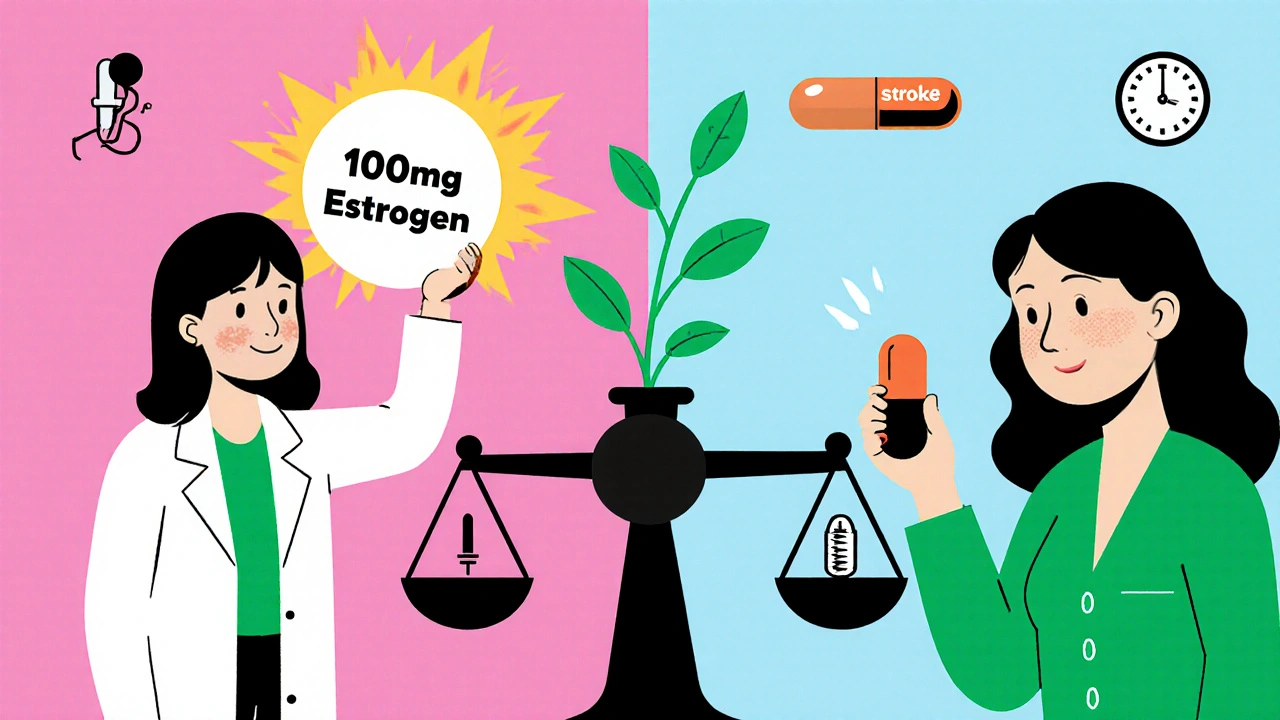
Why Estrogen Makes a Difference
Estrogen in birth control pills, patches, or rings can make your blood more likely to clot. That’s fine for most people. But if you have migraine with aura, your brain is already in a more vulnerable state. The combination of estrogen and migraine with aura raises your risk of ischemic stroke - the kind caused by a blood clot blocking a vessel in the brain.
Here’s what the numbers show: In healthy young women without migraines, the chance of having a stroke in a year is about 6 out of 100,000. If you have migraine with aura and take estrogen-containing birth control, that jumps to around 30 out of 100,000. That’s a fivefold increase. The CDC says the combined risk is six times higher than if you had neither factor. That’s not a small number - it’s enough for global health agencies to warn against it.
What the Guidelines Say - And Why They’re Being Challenged
The World Health Organization (WHO) has been clear since 2015: women with migraine with aura should not use any birth control containing estrogen. The CDC agrees. So do the American College of Obstetricians and Gynecologists (ACOG). These are strong, consistent recommendations.
But here’s the twist: newer research is asking whether those guidelines still make sense today.
Back in the 1970s, birth control pills had 100+ micrograms of estrogen. Today’s pills have 10 to 35 micrograms. Some are as low as 10 micrograms - called ultra-low-dose. A 2022 study led by Dr. Pinar Batur at Cleveland Clinic looked at women with migraine with aura who used modern low-dose pills. The results suggested stroke risk might be much lower than previously thought - especially with doses under 30 micrograms.
Dr. Anne Calhoun, a migraine specialist at Stanford Medicine, argues that the fear around estrogen and migraines comes from outdated high-dose pills. She points out that some low-dose formulations may even reduce the frequency of aura episodes, which could lower stroke risk over time.
But here’s the catch: that 2022 study only included 127 women who had strokes. That’s not enough to change national guidelines. Experts agree: this is one piece of a very complex puzzle. The WHO hasn’t changed its stance. Neither has the CDC. So while the science is evolving, the official advice hasn’t.
Frequency Matters - More Than You Think
Not all migraine with aura is the same. How often you get it changes your risk dramatically.
Studies show:
- If you have aura more than 12 times a year, your stroke risk jumps 10 times higher than someone who doesn’t have migraines.
- If you get aura at least once a week, your risk is over four times higher.
- If you only get aura once a month, the risk doesn’t seem to go up significantly.
- And here’s the most important part: if you haven’t had aura in the past year, your risk returns to baseline. Past aura doesn’t count - only recent, active aura does.
This means your history matters. If you used to get aura every week but haven’t had one in 18 months, your risk profile is very different from someone who gets aura every other day. A doctor needs to know your pattern - not just whether you’ve ever had it.
Other Risk Factors That Multiply the Danger
Migraine with aura alone is risky. But add one more factor - and the numbers get scary.
Smoking. High blood pressure. Diabetes. A family history of stroke. Being over 35. All of these pile on. If you smoke and have migraine with aura, your stroke risk isn’t just doubled or tripled - it’s multiplied. That’s why WHO and ACOG say estrogen-containing birth control is absolutely off-limits for smokers with aura, no matter the dose.
Even if you don’t smoke, if your blood pressure is above 140/90, or if you’ve had a relative with a stroke before age 50, you’re in a higher-risk group. That’s why a simple yes/no answer doesn’t work. Your full health picture matters.
What Are Your Safe Alternatives?
If estrogen birth control isn’t safe for you, that doesn’t mean you have to go without contraception. There are plenty of effective, safe options.
Progestin-only methods are the gold standard for women with migraine with aura. These include:
- Progestin-only pills (POP) - taken daily. Must be taken at the same time every day to be effective.
- Implant (etonogestrel) - a small rod placed under the skin of your arm. Works for up to 3 years.
- Injectable (Depo-Provera) - a shot every 3 months.
- Levonorgestrel IUD - placed in the uterus. Works for 3 to 8 years, depending on the brand. Also reduces menstrual bleeding - which many women with migraines appreciate.
Nonhormonal options are also safe:
- Copper IUD - lasts up to 12 years. No hormones. Just works by creating a reaction in the uterus that stops sperm.
- Condoms, diaphragms, cervical caps - less effective on their own but safe and can be combined with other methods.
These methods don’t raise stroke risk. They’re not just alternatives - they’re recommended.
What Should You Do Right Now?
If you have migraine with aura and are using or thinking about estrogen birth control, here’s your action plan:
- Confirm your diagnosis. Are your symptoms truly aura? Or are they just pre-migraine symptoms like fatigue or mood changes? Ask your doctor to document it.
- Track your attacks. How many a month? How long do they last? When was your last one? Keep a simple calendar or use a migraine app.
- Check your other risks. Do you smoke? Is your blood pressure normal? Do you have a family history of stroke or clotting disorders?
- Ask about progestin-only options. Don’t assume you have to stick with the pill you’re on. Ask your provider: ‘What’s the safest, most effective option for me?’
- Don’t panic, but don’t ignore it. You don’t need to stop your pill tomorrow unless you’re also smoking or have high blood pressure. But you do need to have a real conversation with your doctor - not just a quick refill.
Many women with migraine with aura are told they can’t use hormonal birth control - and then they stop using birth control altogether. That’s not the answer. The answer is finding the right method. Progestin-only options work well. Many women report fewer migraines on them, not more.
The Bottom Line
Migraine with aura and estrogen birth control is a high-risk combo - but not a dead end. The guidelines exist for a reason: the risk is real. But the science is changing. Low-dose estrogen might be safer than we thought. Still, until we have more data, the safest path is clear: avoid estrogen if you have active aura.
Your body, your choices. But make them with full information. Talk to your doctor. Get your aura properly diagnosed. Know your numbers. And don’t settle for a one-size-fits-all answer. There are safe, effective options out there - you just need to ask for them.


Amy Hutchinson
November 25, 2025 AT 06:08i just started taking that low-dose pill last month and my aura’s been worse than ever. like, i saw zigzags during my zoom meeting and my boss thought i was zoning out. turns out i was having a full-blown migraine. why does everyone act like this is just a ‘maybe’? my neurologist told me to ditch estrogen ASAP and i’m still mad i didn’t listen sooner.
Archana Jha
November 26, 2025 AT 08:32soooo… what if the whole ‘estrogen causes strokes’ thing is just a pharma lie? they make billions off iuds and implants. what if low-dose pills are fine but they scared women into buying expensive alternatives? i read a blog where a woman in russia used estrogen for 15 years and never had a stroke. coincidence? or cover-up? 🤔
Sharley Agarwal
November 28, 2025 AT 08:20you’re all overreacting. if you can’t handle a little aura, maybe you shouldn’t be on birth control at all. it’s not rocket science. just stop taking estrogen. done.
prasad gaude
November 29, 2025 AT 07:28in india, we have this saying: ‘the river doesn’t ask the fish if it wants to swim.’ but here, women are being told their bodies are ticking bombs because of migraines. i’ve seen women in my village use the pill for decades and live to 80. maybe the real danger isn’t estrogen-it’s fear dressed up as science.
we need to stop treating women like fragile glass. we’ve survived wars, famines, and patriarchy. can’t we survive a little hormonal tweak?
Srikanth BH
November 30, 2025 AT 12:11hey, if you’re reading this and you’re scared-take a breath. you’re not alone. i had migraine with aura for years and switched to the implant last year. no more aura episodes. no strokes. just peace. it took me 3 doctors and 2 years to find the right fit, but it was worth it. you got this. your health isn’t a compromise-it’s a priority.
Jennifer Griffith
December 2, 2025 AT 00:18wait so if i havent had aura in a year im fine? so like… if i just dont get em for 12 months i can go back on the pill? i thought it was forever??
Patricia McElhinney
December 3, 2025 AT 12:51It is imperative to underscore that the World Health Organization's 2015 guidelines are not suggestions-they are evidence-based mandates grounded in epidemiological consensus. To casually disregard these recommendations based on anecdotal data or underpowered studies is not only medically irresponsible, it is potentially life-threatening. The 30/100,000 statistic is not a suggestion-it is a warning bell. Your autonomy does not supersede the burden of preventable stroke risk.
Rachel Villegas
December 5, 2025 AT 04:23Just wanted to add-my doctor switched me to the Mirena IUD after my last aura episode. My migraines actually got better. No more monthly panic about whether I’m going to lose vision for an hour. And the bleeding? Minimal. I wish someone had told me this sooner. Progestin-only isn’t just safe-it’s a game changer.