Diuretic Overview – What They Are and Why They Matter
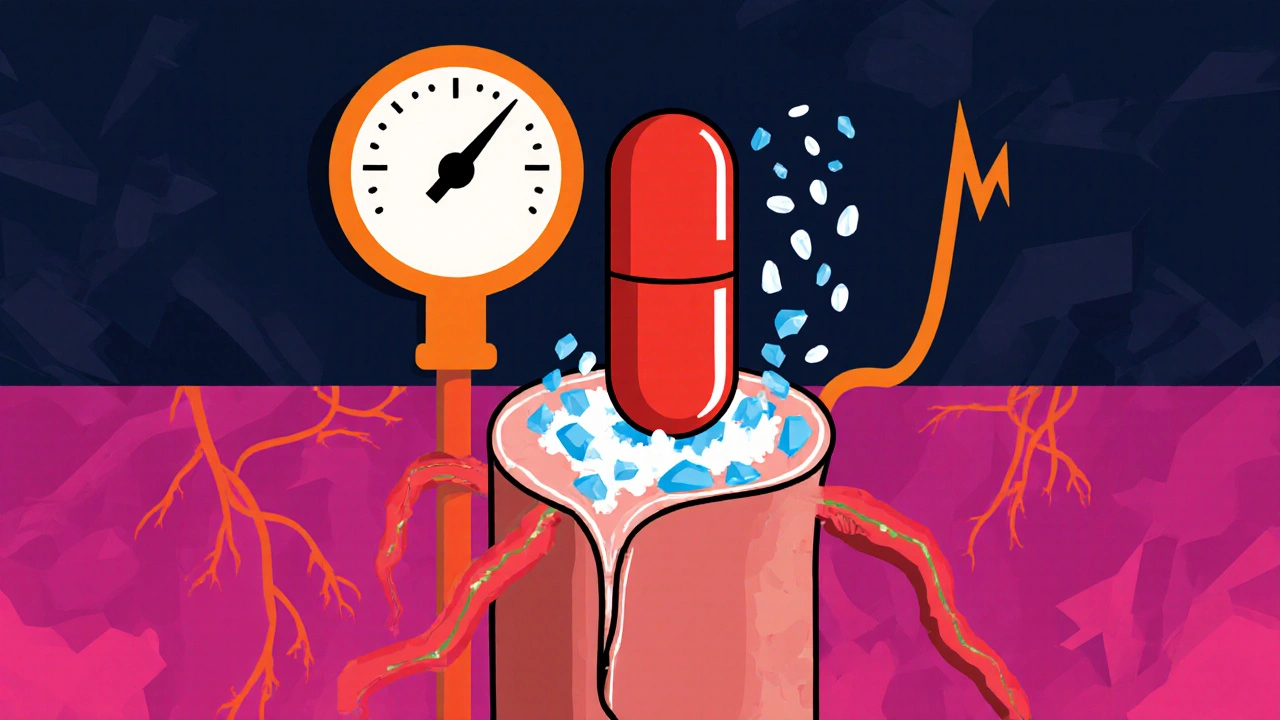
When talking about Diuretic, a medication that helps the body eliminate excess water and salt through urine. Also known as water pill, it reduces fluid buildup and eases pressure on the heart and blood vessels, you’re dealing with a tool that directly impacts Hypertension, high blood pressure that often requires medication to control. The link is simple: more fluid means higher pressure, so pulling fluid out helps lower that pressure. At the same time, removing fluid shifts electrolytes, so Electrolyte imbalance, disruptions in sodium, potassium, and other minerals can be a side effect you need to watch. This trio—diuretic, hypertension, and electrolyte balance—forms the core of what you’ll read about below.
How Diuretics Influence Kidney Function and Blood Pressure
The kidneys act as the body’s filter, and diuretics tell them to let more water pass through. When the kidneys increase urine output, blood volume drops, and the heart doesn’t have to pump as hard. That drop in workload directly diuretic lowers blood pressure, which is why doctors prescribe them for Kidney disease, any condition that impairs kidney’s ability to regulate fluids and electrolytes as well as for heart-related issues. The semantic triple here is clear: diuretics → reduce → blood volume; reduced blood volume → lowers → blood pressure; lower blood pressure → helps → manage hypertension. Understanding this chain helps you see why a simple pill can have big effects on heart health and why monitoring is essential.
There are three main families of diuretics, each working at a different point in the kidney’s tubule system. Loop diuretics act on the thick ascending limb, pulling out large amounts of sodium, potassium, and water—great for fast fluid removal in edema or acute heart failure. Thiazide diuretics target the distal convoluted tubule and are often first‑line for chronic hypertension because they provide a moderate, steady fluid loss. Potassium‑sparing diuretics work farther downstream, ending with less potassium loss, which helps mitigate the electrolyte‑imbalance risk. Choosing the right class depends on the condition you’re treating, your kidney health, and how your electrolytes are holding up.
Safety comes first when using diuretics. Because they change how much salt and water leaves the body, they can cause low potassium (hypokalemia), low sodium (hyponatremia), or even dehydration. Regular blood tests let you catch these shifts early. If you’re already on a blood‑pressure medication, adding a diuretic can enhance the effect, but you might need dose adjustments to avoid an overly low pressure reading. People with severe kidney disease may need a gentler approach or a different drug class altogether. Staying hydrated, eating a balanced diet with enough potassium‑rich foods, and checking in with your healthcare provider are simple steps that keep the benefits outweighing the risks.
Below you’ll find a curated list of articles that dive deeper into specific drugs, conditions, and practical tips. Whether you’re curious about how a particular diuretic compares to others, want to understand the latest research on fluid management, or need guidance on monitoring electrolytes, the collection has you covered. Explore the posts to get detailed comparisons, safety guidelines, and real‑world advice that will help you make informed choices about using diuretics in your health plan.
Amiloride for Salt Sensitivity: How It Can Help Manage High Blood Pressure
Explore how amiloride works, its evidence in salt‑sensitive hypertension, who benefits, dosing tips, side‑effects, and future research in a practical guide.
Read more