When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. But behind that simple expectation is a complex science that’s changed dramatically over the last decade. Quality by Design (QbD) isn’t just a buzzword-it’s now the standard for how generic drugs are developed and approved. Gone are the days when manufacturers simply copied a brand-name drug’s formula and tested the final product for quality. Today, QbD requires understanding every step of the process-before you even make the first batch.
What Exactly Is Quality by Design?
Quality by Design, as defined by the International Council for Harmonisation (ICH) in its Q8(R2) guideline, is a systematic way of building quality into a drug from the start. It means knowing exactly how each ingredient, machine setting, and environmental condition affects the final product. The goal? To make sure every tablet, capsule, or injection performs the same way-every time.
This approach flips the old model on its head. Before QbD, companies relied on testing finished products. If a batch passed lab tests, it was approved. But if it failed, the whole batch was thrown out. That’s expensive and reactive. QbD is proactive. You design the process so failure is unlikely from the beginning.
The U.S. Food and Drug Administration (FDA) made QbD mandatory for all Abbreviated New Drug Applications (ANDAs) submitted after October 1, 2017. That’s not a suggestion-it’s a rule. And it’s working. According to the FDA’s 2022 report, generic drug approvals rose by 23% after QbD became standard, and review times dropped by nearly five months per application.
The Five Pillars of QbD in Generic Drugs
QbD isn’t one big idea-it’s five connected parts that work together. Think of them as the foundation of a house. Skip one, and the whole structure wobbles.
1. Quality Target Product Profile (QTPP)
This is your blueprint. It lists everything the drug must do: how fast it dissolves, how much active ingredient it contains, what impurities it can have, and how stable it is over time. For a generic to be approved, it must match the brand-name drug’s performance within 95% accuracy-especially in dissolution tests. If the brand dissolves 80% of its drug in 30 minutes, your version must do the same.
2. Critical Quality Attributes (CQAs)
These are the measurable features that directly affect safety and effectiveness. For most generic tablets, developers track 5 to 12 CQAs. The big ones? Dissolution rate (must have an f2 similarity factor above 50), content uniformity (no more than 6% variation between tablets), and impurity levels (must stay under ICH Q3B limits). Miss one of these, and your application gets rejected.
3. Critical Process Parameters (CPPs)
These are the settings on your manufacturing equipment that influence CQAs. For example, if you’re making a tablet, CPPs might include: granulation moisture (1.5-3.0%), compression force (10-15 kN), and drying temperature (40-50°C). Too much moisture? Tablets stick together. Too little? They crumble. QbD doesn’t fix these at one point-it defines safe ranges.
4. Design Space
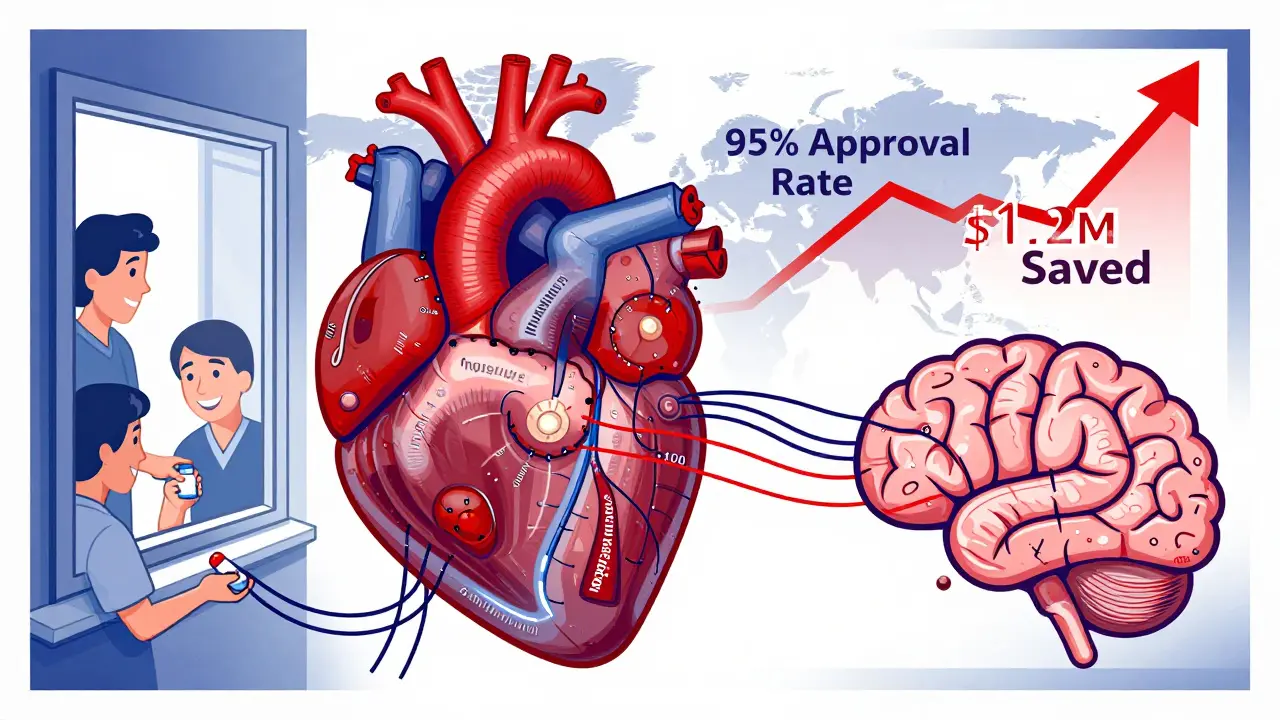
This is where QbD gets powerful. Design space is the set of all possible combinations of CPPs that still produce a high-quality product. It’s not a single setting-it’s a range. The FDA accepts design spaces built on data from 100+ simulated batches, with 95% confidence that the product will meet all CQAs. Once approved, you can tweak parameters within this space without asking for new permission. That saves companies $1.2 million to $2.8 million per product annually in paperwork and delays.
5. Control Strategy
This is how you make sure you stay within the design space. It includes real-time monitoring tools like near-infrared spectroscopy (PAT), which checks tablet composition as they’re being made. Companies using PAT reduce end-product testing by 35-60%. That means faster releases, less waste, and fewer recalls.
QbD vs. Traditional Development: The Numbers Don’t Lie
Let’s compare two ways of making a generic drug.
Traditional Method:
- Fixed recipe: “Mix for 15 minutes at 25°C.”
- Single target for each step.
- No understanding of why a change might break the product.
- High risk of batch failure.
- Approval takes 13.9 months on average.
QbD Method:
- Scientifically proven ranges: “Mix between 12-18 minutes at 22-28°C.”
- Understands how changes affect quality.
- Can adjust parameters without reapproval.
- 28-42% more robust during scale-up.
- Approval takes 9.2 months on average.
The FDA’s Office of Generic Drugs found QbD-based applications get 31% fewer Complete Response Letters (CRLs)-those are the dreaded letters that say “we need more data.” That’s huge. Less back-and-forth means faster access to affordable medicines.

Where QbD Shines-and Where It Struggles
QbD isn’t a one-size-fits-all solution. It works best where complexity is high.
Where it excels:
- Modified-release tablets (delayed or extended action)
- Inhalers and nasal sprays
- Transdermal patches
- Complex injectables
These products have tricky absorption patterns. Traditional bioequivalence tests often can’t predict how they’ll behave in the body. QbD uses advanced in vitro testing to simulate real-world performance, reducing the need for expensive clinical trials.
Where it’s overkill:
- Simple immediate-release tablets (like 500mg paracetamol)
- Low-cost generics with thin margins
For these, the FDA and industry experts warn against “over-engineering.” One case study showed a company spent $450,000 on DoE studies for a drug with a well-known, stable design space. The return? None. The cost? Unnecessary.
Experts like Dr. James Polli from the University of Maryland argue that QbD should be proportionate. Don’t use a sledgehammer to crack a nut.
Real-World Impact: What Companies Are Saying
Companies that have made the switch report real savings and fewer headaches.
Dr. Elena Rodriguez from Hikma Pharmaceuticals said implementing QbD for their generic esomeprazole dropped post-approval deviations from 14 per year to just 2. That saved $850,000 annually in investigations and recalls.
At Mylan (now Viatris), Dr. Sarah Kim used QbD’s design space to make 11 manufacturing adjustments for simvastatin without seeking FDA approval. During pandemic supply chain chaos, that meant 99.8% on-time delivery.
But it’s not all smooth sailing. Dr. Mark Chen from Lupin Limited said the initial training cost 120 hours per scientist-and it disrupted early submissions. Many teams struggled to justify design space boundaries for complex formulations. And 63% of QbD failures, according to the EMA, come from not understanding how the drug behaves in the body-not just in the lab.
How to Implement QbD: A Practical Roadmap
If you’re building a generic drug today, here’s what you need to do:
- Define the QTPP-start with the brand-name drug’s profile.
- Identify CQAs-focus on dissolution, uniformity, impurities.
- Run DoE studies-use statistical experiments to map how CPPs affect CQAs.
- Establish design space-prove it works across 100+ simulated batches.
- Build control strategy-use PAT tools like NIR or Raman spectroscopy.
- Document everything-the FDA expects clear, traceable science.
For immediate-release products, this takes 6-9 months. For complex ones, 12-18 months. You’ll need:
- Scientists trained in Quality Risk Management (ICH Q9) and Design of Experiments (80-120 hours each)
- PAT equipment (minimum $500,000 investment)
- Software like MODDE Pro ($15,000/user/year)
The FDA’s QbD Pilot Program has approved 87 submissions with a 92% first-cycle approval rate-compared to 78% for traditional apps. And free training modules are available through the FDA’s website, completed by over 1,200 industry professionals in 2022.
The Future of QbD: Where It’s Headed
QbD isn’t standing still. The FDA’s new ICH Q14 guideline (effective December 2023) requires more robust analytical data-but rewards it with 40% faster validation. The agency’s Emerging Technology Program has approved all 27 QbD-based continuous manufacturing applications submitted so far.
By 2027, McKinsey predicts 95% of new generic approvals will use QbD. The push is coming from regulators, but also from business sense. Optimized processes lower cost of goods sold by 22%. That’s money back in the system-money that can keep prices low for patients.
But there’s a warning. The Generic Pharmaceutical Association cautions that QbD must be scaled to the product. For a $10-a-year pill, spending $500,000 on development isn’t sustainable. The key is proportionality. Use QbD where it adds value-not everywhere.
Global regulators are catching up. The WHO now includes QbD in its prequalification program. India’s top 10 generic makers invested $227 million in QbD capabilities in 2022. Even with cost pressures, the trend is clear: science, not guesswork, is now the foundation of generic drug approval.
Final Thoughts: Why QbD Matters
Quality by Design isn’t about making generic drugs more expensive. It’s about making them more reliable. It turns a guessing game into a science. It reduces recalls, speeds approvals, and gives manufacturers flexibility to adapt without risking patient safety.
For patients, that means fewer shortages. For pharmacists, fewer questions from worried customers. For manufacturers, fewer regulatory nightmares. And for the system as a whole, a stronger, more resilient supply of affordable medicines.
The days of “copy and test” are over. The future is designed-and it’s working.


Jodi Harding
January 18, 2026 AT 09:22QbD isn't just science-it's a mindset shift. You stop treating pills like magic boxes and start treating them like engineered systems. That’s the real win.
Andrew Qu
January 19, 2026 AT 23:40Exactly. I’ve seen labs waste months chasing batch failures because they didn’t map their design space. Once they adopted QbD, their approval time dropped from 14 to 8 months. No magic, just math.
Robert Davis
January 20, 2026 AT 16:02Oh please. This is just big pharma’s way of making generics more expensive so they can charge more later. They call it ‘science’ but it’s really just a cost-shifting scheme. The FDA’s just another puppet.
Danny Gray
January 21, 2026 AT 07:18Wait, so you’re saying if I make a pill that dissolves 79.8% instead of 80%, it’s a failure? That’s not science-that’s religious dogma. What if the patient doesn’t care about 0.2%? Who decided this was the law?
kenneth pillet
January 22, 2026 AT 03:40the 0.2 matters because it’s not about one pill it’s about millions of pills over years. tiny drifts add up. i’ve seen recalls from 0.3% variation. not drama. just physics.
Aysha Siera
January 23, 2026 AT 15:30QbD is a trap. The FDA and big pharma are using this to lock out small manufacturers. The ‘design space’ is coded language for ‘you need $2M in equipment or stay out.’ This isn’t science-it’s corporate gatekeeping.
Selina Warren
January 24, 2026 AT 20:54It’s not gatekeeping-it’s responsibility. If your pill doesn’t dissolve right, someone’s heart attack meds don’t work. You think it’s about money? It’s about people dying because someone cut corners. Wake up.
Wendy Claughton
January 25, 2026 AT 05:16I get it… I really do. 💙 But I also feel bad for the small labs trying to compete. It’s like being told you need a Ferrari to drive on a dirt road. The system needs to be more… gentle. More proportional. Not every drug needs a particle-size analysis.
Stacey Marsengill
January 25, 2026 AT 15:51You think this is bad? Wait till you see the next phase: AI-driven dissolution modeling. They’re already training neural nets to predict bioequivalence without human trials. Soon, you’ll be on a pill your doctor never even saw. Just a robot and a database deciding if you live or die. And you’ll thank them for it.
Joni O
January 25, 2026 AT 16:06my team did this for a generic metformin last year. spent 6 months on doe. turned out the brand’s dissolution profile was wrong. we fixed it. now our version’s actually better. no one knew. no one cared. but patients felt it. that’s the quiet win.
Jake Moore
January 26, 2026 AT 09:17For simple tablets? Skip the $500k PAT gear. Use a dissolution tester and a spreadsheet. The FDA’s not stupid-they know proportionality. QbD isn’t about over-engineering. It’s about not under-engineering.
Zoe Brooks
January 28, 2026 AT 06:10It’s wild how much of medicine is still guesswork. But QbD? This is the first time I’ve seen generic drug development feel… noble. Like we’re finally treating patients like humans, not cost centers. 🙌
Eric Gebeke
January 28, 2026 AT 15:47They say QbD reduces recalls. But who’s counting? The same people who said the Vioxx recall was an anomaly. You think this system is clean? It’s just a prettier cage. The real problem? Profit-driven regulation. Always has been.