Getting the right dose of medicine for your child isn’t just important-it can be life-saving. A single mistake, like mixing up milliliters and teaspoons, can mean the difference between healing and harm. You’re not alone if this feels overwhelming. Most parents don’t realize how easy it is to mess up a dose, especially when using kitchen spoons or dosing cups that look right but aren’t accurate. The truth? About 7 in 10 parents make at least one dosing error when giving liquid medicine to their kids. But with the right tools and a few simple steps, you can avoid those mistakes for good.
Why Milliliters (mL) Are the Only Unit That Matters
Stop using teaspoons, tablespoons, or any household measuring tools. Even if the label says "1 tsp," that’s not safe. A real teaspoon from your kitchen can hold anywhere from 3.9 to 7.3 milliliters-way off from the standard 5 mL. That’s a 20% to 200% error. For a child, that’s dangerous. A 20% overdose of antibiotics can cause vomiting or diarrhea. A 200% overdose of acetaminophen can lead to liver failure.
The CDC, the American Academy of Pediatrics, and every major children’s hospital now agree: all pediatric liquid medicines must be measured in milliliters (mL) only. No more "teaspoons" or "tablespoons" on labels. That’s because mL is precise, universal, and doesn’t change based on what spoon you grab. If the prescription says "5 mL," that’s exactly 5 mL-no guessing.
Here’s a critical point: 0.5 mL is not the same as 5 mL. That’s a tenfold difference. One is a drop. The other is a full teaspoon. Confusing them has killed children. Always double-check the number and the unit. Read it out loud: "Five milliliters." Not "five teaspoons."
Which Tool Should You Use? Oral Syringes Win Every Time
Not all measuring tools are created equal. Here’s what works best, ranked by accuracy:
- Oral syringes (1-10 mL) - 94% accurate. Best for doses under 5 mL.
- Dosing cups - 76% accurate. Risky for small doses.
- Medication spoons - 82% accurate. Only if labeled in mL.
- Kitchen teaspoons or tablespoons - Never use. Error rate up to 200%.
For doses under 5 mL-like most antibiotics or fever reducers-use an oral syringe. They’re cheap, often free from your pharmacy, and designed for precision. Hold it upright, look at the line at eye level, and slowly push the plunger to the right mark. Don’t rush. If the medicine is thick, like amoxicillin suspension, shake the bottle well before drawing it up.
Dosing cups are okay for older kids who can drink directly from the cup, especially if the dose is 5 mL or more. But if your child spits out medicine, syringes work better. You can gently squirt it into the side of their mouth, near the cheek, not the front. That reduces spitting and gagging.
How to Convert Weight to Dose (It’s Simpler Than You Think)
Many pediatric doses are based on weight: milligrams per kilogram (mg/kg). That sounds complicated, but you don’t need to be a math expert. Here’s the trick:
- Find your child’s weight in pounds (lb).
- Divide that number by 2.2 to get kilograms (kg).
- Use the dose per kg listed on the prescription.
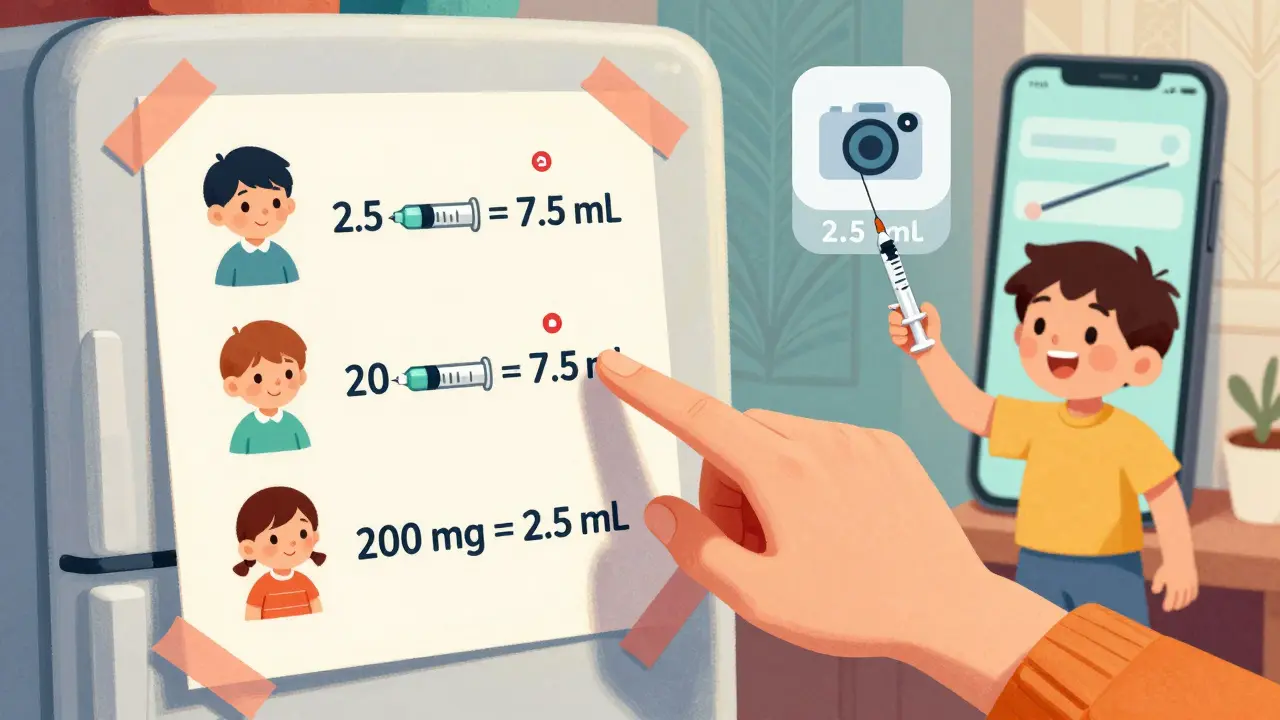
Example: Your 22-pound child needs amoxicillin at 40 mg/kg/day in two doses.
- 22 lb ÷ 2.2 = 10 kg
- 40 mg/kg × 10 kg = 400 mg total per day
- 400 mg ÷ 2 = 200 mg per dose
If the medicine is 400 mg per 5 mL, then 200 mg equals 2.5 mL. That’s your dose. Write it down. Keep it on your fridge. Use a permanent marker to mark your syringe if you give the same dose daily.
Always check the concentration on the bottle. Amoxicillin can be 125 mg/5 mL, 250 mg/5 mL, or 400 mg/5 mL. The dose changes with each. Never assume.

Common Mistakes Parents Make (And How to Avoid Them)
Here are the top errors-and how to fix them:
- Mixing medicine with whole bottles of juice or milk. Your child might not drink it all. They’ll get less than the full dose. Instead, mix with 1-2 teaspoons of applesauce or yogurt.
- Not shaking the bottle. Liquid antibiotics settle. If you don’t shake, the first dose might be too weak, the last too strong. Shake hard for 10 seconds before every dose.
- Using the wrong syringe. Don’t use an insulin syringe (marked in units) or a syringe meant for pets. Use one labeled for children and marked in mL.
- Double-dosing because you’re unsure. If you’re not sure if you gave the dose, don’t give another. Call your pharmacy or doctor. Better safe than sorry.
- Using old medicine. Liquid antibiotics expire fast-usually 14 days after mixing. Check the label. Throw out what’s past its date.
Also, keep a dosing log. Write down the time and dose each time you give medicine. It helps if multiple caregivers are involved. Grandparents, babysitters, or partners might not remember the exact amount.
What to Do If Your Child Refuses the Medicine
Over 60% of parents struggle with this. Your child spits, cries, or turns away. Here’s what works:
- Use a syringe and aim for the cheek pouch, not the tongue. It’s less likely to trigger the gag reflex.
- Chill the medicine (if allowed). Cold can mask bitter tastes.
- Ask your pharmacist for a flavor. Many pharmacies can add cherry, grape, or bubblegum.
- Let your child hold the syringe. Give them control. "You push the plunger. I’ll hold the bottle."
- Offer a reward after. A sticker, a few minutes of a favorite show, or a small snack.
Never force it. Never mix it into a full bottle. Never hide it in food without checking with your doctor first. Some medicines lose effectiveness when mixed with certain foods.
What’s New in Pediatric Dosing (2025-2026)
Things are improving. By 2026, nearly all pediatric liquid medications in Australia and the U.S. will come with a free, pre-filled oral syringe marked only in mL. The FDA is requiring it. Pharmacies are starting to hand them out at discharge.
Some hospitals now use color-coded syringes. Red for antibiotics, blue for fever reducers, green for allergies. It’s a visual cue that reduces errors by 60%. Brands like NurtureShot and Medisana BabyDos are becoming more common in pharmacies.
There are also apps now-like MedSafety-that use your phone’s camera to show you the right level in the syringe. You point it at the bottle, and the app highlights the correct line. It’s not perfect, but it helps.
Still, technology isn’t a replacement for knowing the basics. No app will fix a parent who uses a kitchen spoon. That’s why education matters more than ever.
Who’s Most at Risk-and How to Get Help
Low-income families are over three times more likely to make dosing errors. Why? They often don’t get syringes from the pharmacy. They reuse old cups. They rely on caregivers who don’t speak English well. One in four non-English-speaking parents misreads dosing instructions.
If you’re struggling, ask your pharmacist for help. They have free syringes. They can show you how to measure. Ask for a printed dosing chart. Many hospitals, like Children’s Healthcare of Atlanta, give them out for free. You can also ask your pediatrician for a simple chart based on your child’s weight.
And if you’re ever unsure-call. Don’t guess. Your pharmacist is there for this. So is your doctor. There’s no shame in asking. One question could prevent a trip to the ER.
Measuring medicine correctly isn’t about being perfect. It’s about being careful. It’s about using the right tool. It’s about double-checking. Do that, and you’re doing better than 70% of parents. That’s enough to keep your child safe.
Can I use a kitchen teaspoon if I don’t have a syringe?
No. A kitchen teaspoon is not accurate. It can hold anywhere from 3.9 to 7.3 mL, while a proper teaspoon of medicine is exactly 5 mL. Using it can lead to under- or overdosing. If you don’t have a syringe, call your pharmacy. They’ll give you one for free.
What if the label says "teaspoon" but I have an oral syringe?
Ignore the word "teaspoon" and convert it to milliliters. One teaspoon equals 5 mL. So if the label says "1 tsp," use 5 mL on your syringe. Always trust the mL number, not the household unit.
How do I know if my child got the right dose?
You won’t always know right away. But if your child’s symptoms don’t improve after a few days, or if they get worse-vomiting, rash, drowsiness, or trouble breathing-call your doctor immediately. These could be signs of under- or overdosing. Always follow the full course of antibiotics, even if your child seems better.
Can I reuse an oral syringe?
You can rinse it with clean water and air-dry it between doses. But never use the same syringe for different medicines. Always clean it after each use. If the plunger gets sticky or cracked, throw it away and get a new one. Pharmacies often give out extra syringes if you ask.
Why do some medicines need to be shaken before use?
Many liquid medicines, especially antibiotics, are suspensions. That means the active ingredient settles at the bottom. If you don’t shake it, the first dose might be too weak and the last too strong. Shake hard for 10 seconds before every dose. If the powder doesn’t dissolve completely, call your pharmacist. The medicine might be spoiled.


Jess Bevis
January 28, 2026 AT 12:13Just used a syringe for the first time last week. Game changer. No more guessing. Kid actually took it without crying.
Kathy Scaman
January 29, 2026 AT 13:22I used to use kitchen spoons until my niece almost got hospitalized. Now I keep three syringes in the fridge labeled by medicine. Life’s too short for dosing drama.
Anna Lou Chen
January 30, 2026 AT 19:52Let’s be real - the entire pediatric dosing paradigm is a capitalist construct designed to commodify parental anxiety. The real issue isn’t milliliters versus teaspoons - it’s the medical-industrial complex weaponizing precision to sell you $12 syringes while underfunding public health infrastructure. The fact that we’ve normalized measuring children’s medicine like we’re conducting a lab experiment speaks to our collective alienation from embodied care. Why not just trust intuition? Or ancestral knowledge? Or, I dunno, not giving medicine at all unless absolutely necessary?
Also, color-coded syringes? That’s not innovation - that’s branding masquerading as safety. Next they’ll sell us QR-coded pacifiers that scan your baby’s cortisol levels.
Mindee Coulter
February 1, 2026 AT 01:54Shaking the bottle before each dose is so important I can’t believe people forget. My daughter threw up her whole antibiotic dose because I didn’t shake it. Now I shake it like I’m making a cocktail and I never miss a dose. Syringes are cheap. Just ask for them. Pharmacies love giving them out.
Rhiannon Bosse
February 1, 2026 AT 05:04Okay but have you noticed how every single pediatric medicine label now says "use oral syringe" but no pharmacy ever gives you one unless you specifically ask? That’s not an accident. That’s a trap. They know you’ll use a spoon. They know you’re tired. They know you’re overwhelmed. And they profit from the ER visits that follow. This isn’t about safety - it’s about liability. The system is rigged. I’ve called 12 pharmacies. Only two had syringes. The rest said "we don’t stock them."
And don’t even get me started on the "flavoring" scam. They add sugar and artificial dyes to make it taste better. So now your kid’s getting a dose of medicine AND a sugar bomb. Genius. Thanks, Big Pharma.
Bryan Fracchia
February 1, 2026 AT 15:51I used to stress about this so much until I realized - you don’t need to be perfect, you just need to be consistent. Get one good syringe, write the dose on it with a Sharpie, keep it next to the medicine, and you’re already ahead of 90% of parents. It’s not about being a scientist. It’s about being present. And that’s enough.
Colin Pierce
February 2, 2026 AT 04:25One thing no one mentions: if your kid’s on antibiotics and you’re using a syringe, wipe the tip with a damp cloth after each use. Bacteria builds up fast. I learned that the hard way when my son got a yeast infection from a dirty syringe. Don’t let that happen to you.
Also, if the medicine is thick and gloopy, warm the bottle under running water for 20 seconds before drawing it up. Makes it flow way easier. Just don’t microwave it.
Irebami Soyinka
February 3, 2026 AT 03:22Y’all in US and CA be acting like this is some new science. In Nigeria, we’ve been using syringes since the 80s - because we didn’t have spoons that measured right. We didn’t need a CDC memo to know a teaspoon ain’t a mL. We used what worked. If you don’t have a syringe, go to the market and buy one for 50 naira. Stop waiting for corporations to save you. You got this.
And if your kid spits out medicine? Hold their nose gently. They’ll swallow. Works every time. 😌
doug b
February 3, 2026 AT 21:23My kid used to gag on everything. Then I started giving meds in the cheek pouch like they said - no gagging. No crying. Just quiet. I even got a syringe with a little duck on it. He thinks it’s a toy. I’m not above bribing with duck syringes.