Prescription Drug Workplace Risk Calculator
Calculate Your Workplace Accident Risk
Based on data from the Journal of Occupational and Environmental Medicine (2017), your risk of workplace accidents increases when taking certain medications. Enter your current medications to see how they affect your safety.
Medications and Work Safety: How Prescription Drugs and Hazardous Drugs Impact Job Performance and Workplace Risk
Imagine you’re a nurse preparing chemotherapy for a patient. You’ve worn your gloves, your gown, your mask. But after months of handling these drugs, you start getting rashes you can’t explain. Or maybe you’re a warehouse worker taking painkillers for a back injury, and one morning you feel dizzy lifting a box-just enough to lose your balance. These aren’t rare accidents. They’re everyday risks in workplaces across the country, and they’re tied to two very different kinds of medications: the ones workers take, and the ones they’re exposed to on the job.
The problem isn’t just about being high or drunk. It’s about legal, prescribed drugs that quietly change how your body works-and how safely you can do your job. And it’s not just healthcare workers. Construction crews, factory lines, emergency responders, even office staff on long-term pain meds are affected. The data shows this isn’t hypothetical. In 2023, nearly 8 million U.S. healthcare workers were potentially exposed to hazardous drugs like chemotherapy agents. Meanwhile, 18.7% of workers with chronic pain are on opioids, and 7.2% are on benzodiazepines for stress or anxiety. Combine those two, and your risk of a fall or error jumps by 84%.
Two Sides of the Same Coin
There are two sides to medication-related workplace risk. One side is about what workers take: prescription drugs that slow reaction time, blur vision, or make you drowsy. The other side is about what workers touch, breathe in, or absorb through their skin: hazardous drugs used in hospitals, pharmacies, and labs. These aren’t the same thing, but they both lead to injury, illness, and lost productivity.
On the prescription side, opioids and benzodiazepines are the biggest concerns. Opioids like oxycodone or hydrocodone reduce pain but also dull alertness. Benzodiazepines like lorazepam or diazepam calm nerves but can make you clumsy and slow. A 2017 study in the Journal of Occupational and Environmental Medicine found that workers taking both together were far more likely to have accidents. Even one of them raises the risk of workplace injury by more than double compared to those not taking these drugs.
On the exposure side, it’s the drugs workers handle that become the danger. Antineoplastic agents-chemotherapy drugs-are the most common. NIOSH’s 2024 list includes 267 of them. These aren’t just dangerous to patients. They’re dangerous to the people who mix them, load them, or clean up after them. Exposure happens through tiny droplets in the air, contaminated surfaces, or accidental needle sticks. Skin contact is the most frequent route, accounting for nearly a third of exposures. Inhalation isn’t rare either-almost 4 out of 10 exposures come from breathing in aerosols during drug preparation.
What Happens When You’re Exposed
Acute effects show up fast. Nurses and pharmacists report nausea, vomiting, skin rashes, and hair loss after handling chemotherapy drugs. In 17 documented cases reviewed by OSHA, workers developed these symptoms within hours or days of exposure. But the real danger is what happens over time.
A 2022 CDC meta-analysis of 47 studies found that healthcare workers regularly exposed to hazardous drugs had 2.3 times the risk of reproductive problems-miscarriages, birth defects, infertility. That’s not a small number. It’s a pattern. And it’s not just women. Men exposed to these drugs also show reduced sperm quality.
Cancer risk is even more alarming. A 2022 OSHA review of 12 long-term studies showed healthcare workers handling antineoplastic drugs had 3.4 times higher rates of certain cancers, especially leukemia and bladder cancer. That’s not a guess. That’s data from workers who spent years in oncology units, pharmacies, and surgical centers without adequate protection.
And it’s not just cancer. Chronic exposure to low doses of these drugs can damage organs-liver, kidneys, bone marrow-without obvious symptoms until it’s too late. That’s why surface contamination matters. Even if you don’t feel sick, traces of the drug on a counter, a drawer handle, or your gloves can add up over months and years.

Controls That Actually Work
There’s good news: we know how to stop this. But it takes more than just telling people to wear gloves.
The most effective solution is engineering controls. Closed-system transfer devices (CSTDs) are one of the biggest advances. These are special connectors and needles that prevent drugs from escaping into the air or onto surfaces during mixing and transfer. WorkSafeBC’s 2021 field tests showed CSTDs cut surface contamination by 94.7%. Mayo Clinic’s program, which added CSTDs, better ventilation, and training, reduced exposures by 89% in just two years.
Administrative controls matter too. Training isn’t optional. USP Chapter 800 requires 16 to 24 hours of initial training and 4 to 8 hours every year. But many facilities skip it. A 2021 CDC study found that 43% of workers didn’t properly put on or take off PPE-gloves, gowns, eye protection-even when they had them. Why? Because they were rushed, overworked, or never taught correctly.
And then there’s ventilation. Nearly a third of healthcare facilities have inadequate air flow in areas where hazardous drugs are handled. That means toxic particles linger in the air longer than they should. Air sampling in 2022 showed detectable drug levels in 68% of work areas-even in places that thought they were following protocols.
The Gap Between Policy and Practice
Here’s the uncomfortable truth: rules exist, but they don’t cover everyone.
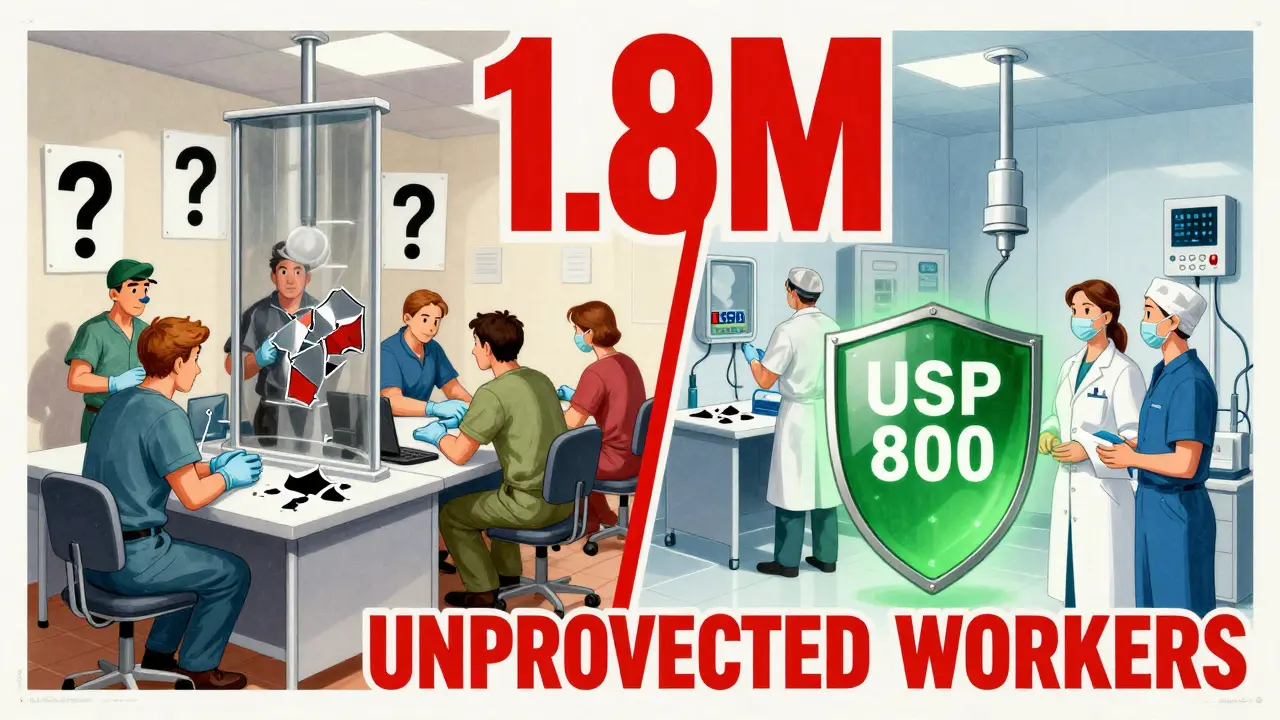
OSHA’s Hazard Communication Standard (29 CFR 1910.1200) only applies to about 6.2 million U.S. workplaces. That leaves 1.8 million healthcare workers-mostly in small clinics, home care, and outpatient centers-without federal protection. They might have gloves, but they don’t have mandatory training, air monitoring, or exposure limits.
USP Chapter 800, which sets stricter standards for compounding pharmacies, only protects around 58,000 workers. That’s a fraction of the 8 million who handle hazardous drugs. Oncology units in hospitals? Not covered by USP 800. Ambulatory surgery centers? Not covered. Even though they’re mixing the same drugs.
And then there’s the issue of workers on prescription meds. Drug-free workplace policies sound good, but they often punish people who need medication. A 2021 editorial in the Journal of Occupational Rehabilitation found that 32% of workers lost their jobs because they took legally prescribed opioids-even when they showed no signs of impairment on the job. That’s not safety. That’s discrimination.
Real Stories, Real Consequences
One chemotherapy nurse on Reddit shared how she developed chronic skin rashes after three years on the job. Despite following all protocols, surface tests showed hazardous drug residue on 68% of surfaces in her unit. She had to switch roles.
An anesthesiologist on Medscape described feeling dizzy and nauseous after taking opioids for a work-related back injury. He nearly caused a surgical error during a procedure. He stopped taking the pills-but lost his ability to work long hours.
But there are wins too. A pharmacy technician on WorkCompWire said after her facility adopted NIOSH’s 2024 guidelines, surface contamination dropped from 42% to 4.7% in six months. Unionized workers reported 22% fewer medication-related incidents than non-union staff. It’s not magic. It’s policy, training, and accountability.
What Needs to Change
Right now, we’re treating this like a compliance issue. It’s not. It’s a public health crisis.
We need OSHA to set a legal exposure limit for hazardous drugs. The proposed limit of 0.1 ng/cm² is a start, but it’s not yet law. We need all healthcare facilities-not just big hospitals-to follow USP 800. We need mandatory air and surface testing in every unit that handles chemotherapy. And we need to stop punishing workers for taking necessary medication.
Employers should be doing risk assessments using NIOSH’s five-step process: identify the drugs, test for exposure, install controls, check if they work, and keep records. But only 78% of large hospitals have full programs. Only 34% of small clinics do.
And we need to stop pretending that “just wear gloves” is enough. Gloves tear. Aerosols spread. Surfaces get missed. We need better technology, better training, and better support for workers who are caught between needing pain relief and staying safe on the job.
The Cost of Doing Nothing
The financial toll is staggering. Occupational medication incidents cost $4.7 billion a year in the U.S.-$2.1 billion in medical bills, $1.8 billion in lost work time, and $800 million in workers’ comp claims. That’s not just numbers. That’s families losing income, hospitals paying higher insurance premiums, and workers forced into early retirement.
The market for safety equipment is growing fast-projected to hit $3.8 billion by 2028. That’s because people are finally seeing the cost of ignoring this problem. But money won’t fix it alone. You can buy the best CSTDs in the world, but if your staff doesn’t know how to use them-or if they’re too tired to follow protocol-nothing changes.
The future is in AI. Johns Hopkins is testing systems that predict high-risk moments during drug handling using real-time sensors. Early results show 92% accuracy. That’s promising. But tech alone won’t solve human factors: fatigue, stress, lack of training, fear of reporting.
The real solution is culture. It’s about making safety part of the job-not an extra step. It’s about listening to nurses who say their gloves are ripping too often. It’s about giving workers time to train properly. It’s about recognizing that someone on opioids isn’t a liability-they’re someone who needs support, not punishment.
What You Can Do
If you’re an employer: audit your drug handling areas. Test surfaces. Ask your staff what they’re seeing. Don’t assume compliance. Test it. Invest in CSTDs. Offer mental health support so workers don’t turn to benzodiazepines for stress. Review your drug policy. Is it protecting safety-or punishing people for being injured?
If you’re a worker: know your rights. Ask for training. Report contamination. Don’t hide symptoms. If you’re on opioids or benzodiazepines, talk to your doctor about alternatives. Can you switch to non-opioid pain relief? Can you get counseling instead of sedatives? Your safety matters more than your silence.
If you’re a policymaker: expand OSHA coverage. Make USP 800 mandatory for all healthcare settings. Fund training programs for small clinics. Stop letting loopholes protect profits over people.
This isn’t about fear. It’s about responsibility. Medications save lives. But they can also end them-if we don’t handle them right.
Can taking prescription painkillers at work really cause accidents?
Yes. Workers taking opioids or benzodiazepines are 2.1 times more likely to suffer a workplace injury than those not taking these drugs. The risk jumps to 84% higher for those taking both together, according to a 2017 study in the Journal of Occupational and Environmental Medicine. These drugs slow reaction time, reduce coordination, and cause drowsiness-all critical for jobs involving machinery, driving, or surgery.
Which healthcare workers are most at risk from hazardous drugs?
Oncology nurses, pharmacists, pharmacy technicians, and staff in ambulatory surgery centers face the highest exposure. These roles handle chemotherapy drugs daily. NIOSH’s 2024 list identifies 267 antineoplastic agents as hazardous, and CDC data shows 28% of exposures occur in oncology units, 32% in pharmacies, and 19% in surgical centers. Even housekeeping staff cleaning these areas are at risk if protocols aren’t followed.
Are gloves enough to protect against hazardous drug exposure?
No. Gloves are just one layer of protection. Skin contact with contaminated surfaces accounts for 22% of exposures, and inhalation of aerosols makes up another 38%. Many gloves aren’t rated for chemotherapy drugs and can tear during use. The CDC found that 43% of workers don’t properly don or doff PPE-even when they have it. Engineering controls like closed-system transfer devices reduce contamination by over 90%, which gloves alone cannot do.
Why aren’t all healthcare facilities required to follow USP Chapter 800?
USP Chapter 800 only legally applies to compounding pharmacies. Hospitals, clinics, and outpatient centers aren’t required to follow it unless state law mandates it. This leaves over 1.8 million healthcare workers unprotected. OSHA’s Hazard Communication Standard covers some aspects but doesn’t address specific hazardous drug handling. This gap means safety depends on where you work-not on what you’re exposed to.
Can workers be fired for taking prescribed medications?
Yes, in many cases. Despite legal protections under the ADA, drug-free workplace policies often lead to termination if a worker tests positive for opioids or benzodiazepines-even if they have a valid prescription and show no impairment. A 2021 study found 32% of workers lost their jobs due to necessary medication use, despite no safety incidents. This creates a dangerous dilemma: take needed medication and risk your job, or go without and risk your health.
What’s the most effective way to reduce hazardous drug exposure?
The most effective method is using closed-system transfer devices (CSTDs), which reduce surface contamination by 94.7% according to WorkSafeBC’s 2021 tests. When combined with proper ventilation, regular air and surface testing, and mandatory training, exposure rates drop by up to 89%. Mayo Clinic’s program, which implemented all these measures, saw the most dramatic results. No single solution works alone-only a layered approach does.
Are new cancer drugs safer for workers?
Not necessarily. In 2023, 42% of newly approved oncology drugs had no established occupational exposure limits. Many are biologics or targeted therapies with unknown long-term effects on workers. NIOSH updates its hazardous drug list annually, but the process is slow. Just in February 2024, two drugs (liraglutide and pertuzumab) were removed from the list after new safety data emerged-showing how quickly science changes, but how slowly policy catches up.


Mike Rose
February 1, 2026 AT 00:37gloves? training? cstds? bro, just fire the ones who can't handle it.
Russ Kelemen
February 2, 2026 AT 23:47People aren't liabilities because they take meds-they're people trying to survive.
And workers handling chemo? They're heroes who don't get paid enough to risk their fertility or get cancer.
We treat safety like a checklist, not a covenant.
Imagine if your job slowly poisoned you and the company said, 'wear gloves' and called it a day.
That's not management. That's negligence dressed up as policy.
Real safety means listening when someone says their gloves tear every shift.
It means paying for training even if it cuts into profit margins.
It means not firing someone because they're on painkillers after a work injury.
That's not safety-that's cruelty.
We need systems that protect people, not just paperwork that protects corporations.
It's not complicated. It's just hard. And hard is better than dead.
Diksha Srivastava
February 3, 2026 AT 13:41Thank you for writing this-people need to know it's not just 'over there' in big hospitals.
Small teams like mine are doing our best with nothing.
Let's push for change together 💪❤️
Sidhanth SY
February 3, 2026 AT 23:29Take a pill to fix the pain? Cool.
Now go back to lifting 50-pound boxes.
Handle chemo? Sure, just wear the same gloves you used yesterday.
We don't fix the system-we fix the person.
And that's backwards.
Maybe if we stopped asking people to choose between their health and their job, we wouldn't have so many accidents.
Just a thought.
Sheila Garfield
February 5, 2026 AT 15:01Turns out the cleaning crew was using the same mops in chemo and non-chemo rooms.
It wasn't malice. Just... ignorance.
Training saved his skin. But why did it take a rash to start listening?
Shawn Peck
February 7, 2026 AT 10:00WE LET PEOPLE TAKE OPIOIDS AND THEN WON'T FIRE THEM?
YOU WANT TO WORK? THEN BE CLEAN.
NO EXCUSES.
IF YOU CAN'T HANDLE YOUR JOB WITHOUT DRUGS, QUIT.
THIS ISN'T A NURSERY.
WE NEED TO STOP CUSHIONING EVERYONE.
GET STRONG. GET CLEAN. OR GET OUT. 🇺🇸
Niamh Trihy
February 8, 2026 AT 10:07Workers don't report rashes or dizziness because they're afraid they'll lose their jobs.
Or worse-they're told it's 'just stress.'
But the data doesn't lie.
And the fact that USP 800 only covers a fraction of workers? That's not oversight. That's systemic abandonment.
We need enforceable standards, not suggestions.
And we need to stop treating workers like collateral damage.
Sarah Blevins
February 10, 2026 AT 03:28Correlation does not imply causation.
Additionally, the financial figures cited are extrapolated from industry estimates, not peer-reviewed longitudinal analyses.
Without a controlled cohort study, this remains anecdotal.
Jason Xin
February 10, 2026 AT 20:35Let me get this straight-workers are punished for taking meds they need... but the people who *expose* them to cancer-causing chemicals get a pass?
That's not a policy gap. That's a moral collapse.
Yanaton Whittaker
February 12, 2026 AT 14:29This isn't danger. This is people being soft.
Wear the gloves. Do the training. Stop crying.
If you can't handle your job, get a new one.
America doesn't need coddling. It needs grit. 💪🇺🇸