When your doctor orders liver function tests, it’s not because they think you’re drinking too much or eating too much fried food. It’s because something in your blood is sending a quiet alarm. These tests don’t measure how well your liver is working like a machine. They measure the leakage of its parts - and that’s where the real story begins.
What You’re Actually Measuring
Liver function tests - or LFTs - are a misnomer. They don’t test liver function. They test liver damage. Think of your liver like a factory. When the walls crack, chemicals spill out into the bloodstream. ALT, AST, ALP, GGT, bilirubin, albumin, and PT are those spilled chemicals. The goal isn’t to see if the factory is making products - it’s to find out if it’s falling apart.
ALT (alanine aminotransferase) is mostly found in liver cells. When those cells die - from virus, fat, toxin, or lack of blood flow - ALT pours into your blood. AST (aspartate aminotransferase) is also in the liver, but it’s everywhere else too: heart, muscles, kidneys. That’s why a high AST could mean a heart attack, not liver trouble. Bilirubin is the yellow waste from broken-down red blood cells. Your liver normally processes it and flushes it out in bile. If it builds up, your skin turns yellow - jaundice.
The Numbers That Matter
Reference ranges vary by lab, but here’s what’s generally accepted in Australia and the US:
- ALT: 7-55 U/L (higher in men, higher in people with obesity)
- AST: 8-48 U/L
- Bilirubin (total): 3-17 μmol/L
- ALP: 40-129 U/L
- Albumin: 35-50 g/L
But here’s the catch: 10-15% of healthy people have ALT or AST levels just above the normal range - and nothing’s wrong. A level of 60 U/L doesn’t mean cirrhosis. It might mean you’re overweight, had a hard workout, or took ibuprofen for a week. That’s why context matters more than the number.
Patterns Tell the Real Story
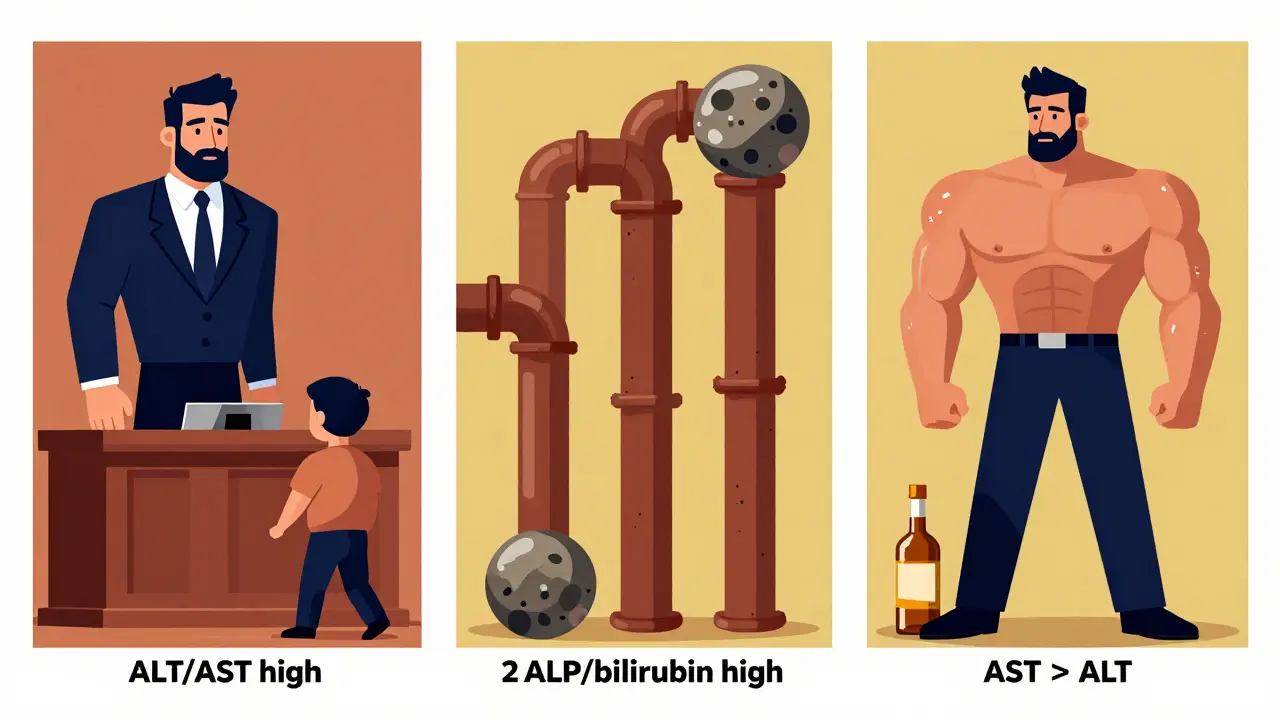
Doctors don’t look at one number. They look at the pattern.
Pattern 1: ALT and AST high, bilirubin and ALP normal or only slightly up
This is hepatocellular injury - liver cells are dying. The bigger the ALT compared to AST, the more likely it’s viral hepatitis or fatty liver. In acute hepatitis A or B, ALT can spike to 1,000 U/L or more. In fatty liver disease (now called MASLD), ALT is usually 1.5 to 2 times higher than AST. If ALT is over 10 times the upper limit, think: viral infection, drug overdose (like paracetamol), or lack of blood flow to the liver.
Pattern 2: ALP and bilirubin high, ALT and AST only mildly up
This is cholestasis - bile isn’t flowing. Something’s blocking the ducts: gallstones, tumors, or medication. ALP can rise 3-10 times normal. But if ALP is high and GGT is normal, look elsewhere - maybe your bones. ALP comes from bone too. A broken rib or bone cancer can trick you.
Pattern 3: AST higher than ALT
This is the alcohol clue. If AST is twice as high as ALT - or more - alcohol is the likely culprit. In alcoholic hepatitis, AST is often 2-6 times normal, while ALT is only 1-2 times. That ratio is more than 90% accurate for alcohol-related damage. But if AST is above 500 U/L, don’t assume it’s just alcohol. Think acetaminophen overdose - especially if the person drank heavily.
Albumin and PT: The True Function Test
Here’s where you see if the liver is still doing its job. Albumin is a protein made by the liver. It keeps fluid in your blood vessels. If albumin drops below 35 g/L, your liver has been struggling for months - maybe years. It’s not a quick signal. Albumin’s half-life is 20 days. A low level means chronic damage: cirrhosis, long-term alcohol use, or severe malnutrition.
Prothrombin time (PT) measures how fast your blood clots. The liver makes clotting factors. If PT is prolonged, your liver can’t make them fast enough. This is urgent. A rising PT means acute failure - maybe from drug toxicity or severe hepatitis. It’s a red flag. A normal PT with low albumin? That’s chronic. A high PT with normal albumin? That’s sudden and dangerous.
What Doesn’t Show Up
Many people think if their LFTs are normal, their liver is fine. That’s not true. In early cirrhosis, ALT and AST can be normal or only slightly raised. The liver is scarred, but not leaking much. The real damage is hidden. That’s why doctors now use FIB-4 or APRI scores - blood tests that combine age, platelets, ALT, and AST to estimate scarring. A 2021 study showed combining these with LFTs boosted accuracy for advanced liver disease from 68% to 89%.
And then there’s GGT. It’s not part of the classic panel, but it’s often checked. GGT rises with alcohol, bile duct problems, or even just being overweight. Isolated GGT elevation? It’s common in metabolic syndrome. But it’s not specific. A high GGT with normal ALT? Could be nothing. Could be early fatty liver. Could be a sign to cut back on wine.
When to Worry - And When to Wait
Not every elevated LFT needs a scan or a specialist. Here’s what most doctors do:
- ALT or AST under 80 U/L? Wait 3 months. Repeat. Check weight, alcohol, meds, diabetes. No need for ultrasound yet.
- ALT or AST over 500 U/L? Refer immediately. Could be drug overdose, acute viral hepatitis, or ischemic injury.
- ALT rising more than 100 U/L per week? That’s fast. Needs urgent review.
- Albumin below 35 g/L or PT prolonged? Refer to liver specialist. This isn’t mild.
- Isolated bilirubin high? Check for Gilbert’s syndrome - a harmless genetic condition that causes mild jaundice under stress.
And here’s a hard truth: 37% of GPs order ultrasounds or CT scans for ALT levels between 41-80 U/L - even when there’s no other sign of disease. That’s over-testing. It adds cost, anxiety, and radiation - for no benefit.
What You Can Do
If your LFTs are off:
- Stop alcohol completely - even if you think it’s “just a few drinks.”
- Check your medications. Some painkillers, antibiotics, and supplements (like green tea extract or high-dose niacin) can damage the liver.
- Manage your weight. Losing 5-10% of body weight can reverse fatty liver.
- Control blood sugar. Type 2 diabetes and fatty liver go hand-in-hand.
- Don’t panic. Most mild elevations improve with lifestyle changes.
And if your numbers are normal? Don’t assume you’re safe. Fatty liver can be silent for years. Get checked if you’re overweight, diabetic, or drink regularly - even if your tests are fine now.
What’s Next?
The future of liver testing isn’t just ALT and AST. New blood tests like the ELF test (Enhanced Liver Fibrosis) measure collagen fragments to detect scarring before it’s visible on ultrasound. In 2024, studies showed these tests catch advanced fibrosis with 92% accuracy when combined with AST/ALT ratios.
But the best tool is still you - paying attention to your body, your habits, and your numbers. The liver doesn’t shout. It whispers. And if you listen - with the right tests and the right questions - you can hear it before it breaks.
Can normal liver function tests mean I don’t have liver disease?
Yes. Early cirrhosis or fatty liver can have normal ALT and AST levels. The liver can be scarred or full of fat without leaking enzymes. That’s why doctors use other tools - like FIB-4 scores, ultrasound, or elastography - to check for hidden damage, especially if you’re at risk from obesity, diabetes, or alcohol.
Why is AST higher than ALT in alcohol-related liver disease?
Alcohol damages liver cells differently than viruses or fat. It causes mitochondrial damage, which releases more AST than ALT. AST is also found in muscle, and heavy drinkers often have muscle breakdown from poor nutrition or alcohol toxicity. The result? AST rises more than ALT - often twice as high. That ratio is one of the most reliable clues for alcohol-related injury.
Can exercise raise ALT and AST?
Yes. Strenuous exercise, especially weightlifting or endurance training, can cause muscle damage, which releases AST into the blood. ALT can rise too, though less often. If you’ve had a hard workout, wait 48 hours before getting tested. A sudden spike after exercise is normal - but if it stays high for weeks, that’s a red flag.
What causes isolated bilirubin elevation?
The most common cause is Gilbert’s syndrome - a harmless genetic condition affecting about 5% of people. The liver can’t process bilirubin efficiently under stress (fasting, illness, fatigue). It causes mild jaundice, especially in the morning, but no liver damage. No treatment is needed. Other causes include bile duct blockage, hepatitis, or certain medications.
How long does it take for ALT to return to normal after liver damage?
ALT has a half-life of about 47 hours - meaning it takes roughly 2-3 weeks to drop to normal after the injury stops. AST clears faster, in about 5-7 days. That’s why ALT is better for tracking recovery. If ALT stays high after 3 months, the damage is likely ongoing - and needs investigation.
Can I reverse liver damage shown by abnormal LFTs?
Yes - if caught early. Fatty liver, early inflammation, and even mild fibrosis can reverse with weight loss, stopping alcohol, controlling blood sugar, and avoiding liver-toxic drugs. The liver is the only organ that can regenerate. But once cirrhosis sets in, scarring is permanent. The goal then is to stop it from getting worse.


caroline hernandez
February 3, 2026 AT 13:44Let’s be real-ALT and AST are just the canaries in the coal mine. The real red flag isn’t the number, it’s the pattern. If your AST is double your ALT and you’re sipping wine while scrolling TikTok at 2 a.m., that’s not ‘social drinking,’ that’s a liver screaming for help. And don’t even get me started on people who think green tea extract is ‘natural’ so it’s safe. Nope. It’s a silent hepatotoxin. Context is king.
Sherman Lee
February 4, 2026 AT 08:06They’re lying to you. 🤫 The ‘normal’ ranges? Made by Big Pharma to make you feel fine while your liver turns to mush. I checked my labs after 3 months of juicing-ALT was 68. Docs said ‘it’s fine.’ I went to a naturopath. Turned out I had early-stage NAFLD from ‘healthy’ agave syrup. They don’t want you to know. 🍃💀
Coy Huffman
February 5, 2026 AT 22:43hmm… so the liver’s like a factory that leaks when it’s tired? kinda makes sense. i always thought it was just about drinking, but turns out my 3am ramen binges and stress-sleeping are probably worse. i mean, if it’s not shouting, it’s just whispering… and i’ve been ignoring it. 😅
Demetria Morris
February 7, 2026 AT 01:19It’s pathetic how many people treat their bodies like disposable machines. You don’t need a blood test to know that binge drinking, sugar, and 10-hour workdays are destroying you. If your liver’s leaking, it’s because you’ve been negligent for years. No miracle cure. Just stop. Now.
Geri Rogers
February 8, 2026 AT 11:04YES. 🙌 I’m a nurse and I see this every day. People panic over an ALT of 55, then ignore the 120 lb weight gain, the daily soda habit, and the 6-packs on weekends. But guess what? Lose 10% of your body weight, cut out alcohol, and you’ll see your numbers drop like magic. Your liver is a superhero-it can heal. You just gotta let it. 💪❤️
Samuel Bradway
February 10, 2026 AT 03:42man i had a weird spike last year after a marathon. thought i was dying. turned out it was just muscle damage. waited a month, retested-back to normal. point is, don’t freak out over one number. context, context, context. and yeah, i do drink. but i don’t do it every night. that’s the line, right?
Jamillah Rodriguez
February 10, 2026 AT 16:39so like… if my ALT is 58 and I’m 32 and I eat avocado toast… is that the end? 😭 i’m just trying to live my best life. also why does everyone act like liver damage is some secret cult? it’s just… biology. 🤷♀️
Susheel Sharma
February 12, 2026 AT 00:42Let me dissect this with surgical precision. The assertion that ALT/AST ratio is 90% accurate for alcohol-related injury is statistically misleading. Studies show a 12% false-positive rate in non-alcoholic steatohepatitis patients with concurrent metabolic syndrome. Furthermore, GGT elevation in South Asian populations correlates more strongly with insulin resistance than alcohol intake-yet Western guidelines ignore this. This is not medicine. It’s colonial diagnostics.
Janice Williams
February 12, 2026 AT 08:52How dare you suggest that elevated liver enzymes might be benign? This is irresponsible. The liver is sacred. If your numbers are off, you are morally compromised. You have chosen poor hygiene, poor discipline, and poor character. This is not a medical issue-it is a spiritual failure. I have seen the data. The truth is not comfortable. But it is necessary.
Shelby Price
February 14, 2026 AT 02:00so wait… if i have gilbert’s syndrome and my bilirubin is high but everything else is normal… does that mean i’m just kinda… naturally yellow? 🤔
Jesse Naidoo
February 14, 2026 AT 07:06you guys are all missing the point. i got my numbers checked after my divorce. everything was normal. but i felt awful. i cried every day. turns out, my liver was fine. my soul was broken. why do we only fix bodies? why not fix hearts? 🥺
Daz Leonheart
February 15, 2026 AT 07:25you got this. even if your liver’s been through hell, it can bounce back. i lost 40 lbs, quit soda, started walking 30 mins a day. 6 months later, my alt dropped from 82 to 39. it’s not magic. it’s just showing up. you don’t need a fancy test. you just need to care. 💪
Amit Jain
February 16, 2026 AT 04:27simple: if you drink, eat junk, sit all day-your liver will suffer. no need for big words. stop bad habits. move more. eat real food. liver will fix itself. easy.