Statins save lives. Millions of people take them every day to lower cholesterol and prevent heart attacks and strokes. But for some, the cost is muscle pain - sometimes severe enough to stop the medication entirely. The real danger isn’t just the statin itself. It’s what happens when it mixes with other drugs. That’s where the risk of myopathy spikes - a condition that can turn mild discomfort into life-threatening muscle breakdown.
What Exactly Is Statin-Induced Myopathy?
Myopathy means muscle disease. In the context of statins, it’s when your muscle fibers start breaking down. You might feel sore, weak, or crampy - like you’ve run a marathon without ever leaving the house. But here’s the catch: not all muscle pain from statins is the same. Most cases are mild and don’t show up in blood tests. But when creatine kinase (CK) levels rise more than 10 times the normal upper limit, that’s clinical myopathy. And if it gets worse? That’s rhabdomyolysis - muscle tissue melting into your bloodstream, potentially wrecking your kidneys.The good news? Rhabdomyolysis is rare. Even with drug interactions, it happens in less than 1 in 10,000 people per year. The bad news? It’s preventable. And too often, it’s not caught until it’s too late.
Not All Statins Are Created Equal
If you’re on a statin and having muscle issues, switching might be easier than you think. Statins vary wildly in how they’re processed by your liver - and that changes your risk.- High-risk statins: Simvastatin and lovastatin are mostly broken down by the CYP3A4 enzyme. That means anything that blocks this enzyme - like certain antibiotics or heart meds - can cause statin levels to skyrocket.
- Moderate-risk: Atorvastatin is also partly processed by CYP3A4, so interactions still matter, but less so.
- Low-risk statins: Pravastatin, rosuvastatin, and fluvastatin don’t rely heavily on CYP3A4. They’re cleared through other pathways, making them much safer when combined with other drugs.
Here’s the kicker: studies show muscle pain rates vary from 0.6% with pravastatin to over 12% with rosuvastatin. That’s not a typo. Rosuvastatin’s higher incidence isn’t because it’s more dangerous - it’s because it’s more potent. Higher doses mean more muscle exposure. But even then, pravastatin remains the safest bet when interactions are a concern.
The Big Three Drug Interactions That Raise Myopathy Risk
Some medications are silent killers when paired with statins. They don’t cause problems on their own - but together? They turn your statin into a muscle toxin.1. Macrolide Antibiotics
Clarithromycin and erythromycin are common for sinus infections and pneumonia. They block CYP3A4 - and they’re not gentle about it. Clarithromycin can spike simvastatin levels by 10 times. Atorvastatin? Up by 4 times. That’s enough to push someone into myopathy territory.Azithromycin? Totally different story. It doesn’t touch CYP3A4. If you need an antibiotic and you’re on a statin, ask for azithromycin. It’s just as effective, and it won’t wreck your muscles.
2. Fibrates
Gemfibrozil is the worst offender. It doesn’t just interfere with metabolism - it blocks the liver’s ability to clear statins from your blood. Studies show it can double statin levels. Fenofibrate? Much safer. If you’re on both a statin and a fibrate for mixed lipid issues, go with fenofibrate. Avoid gemfibrozil unless there’s no other option.3. Immunosuppressants and Heart Meds
Cyclosporine - used after transplants - can increase statin levels by up to 13 times. That’s why transplant patients on statins are often put on pravastatin or fluvastatin at low doses.Diltiazem, verapamil, and amiodarone? All raise statin levels. The FDA actually limited simvastatin to 20mg max if you’re on any of these. That’s not a suggestion - it’s a safety rule. And even then, the risk stays elevated.

Who’s Most at Risk?
It’s not just about the drugs. Your body matters too. Seven key factors make muscle damage more likely:- Age over 75
- Small body frame or low BMI
- Chronic kidney disease
- Hypothyroidism
- Heavy alcohol use
- Intense exercise (especially if you’re not used to it)
- Being on multiple interacting drugs
Think of it like this: if you’re a 78-year-old woman with underactive thyroid, taking simvastatin 40mg and diltiazem, and you just started a new walking program? You’re in the danger zone. Not because you’re doing anything wrong - but because the combination is toxic.
What Should You Do If You Have Muscle Pain?
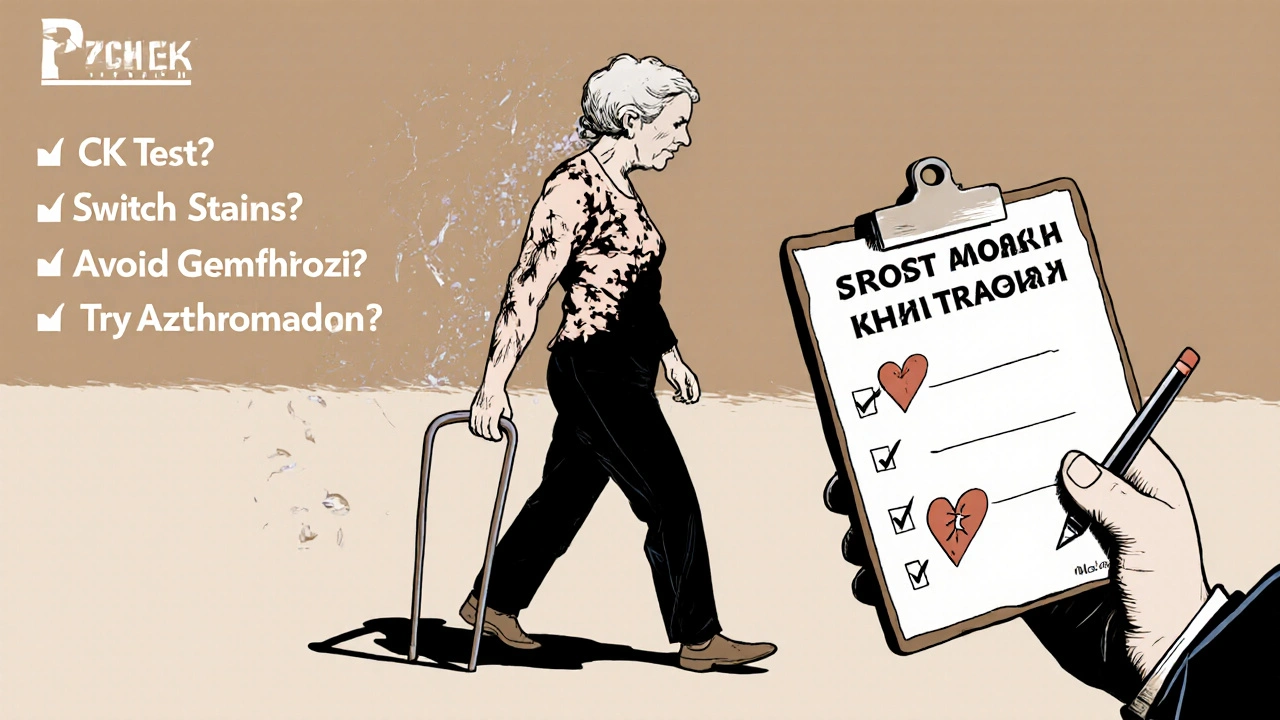
Don’t ignore it. Don’t assume it’s just aging. Don’t stop the statin without talking to your doctor.Here’s the step-by-step:
- Check your meds. Look at every prescription, over-the-counter pill, and supplement. Even St. John’s Wort or grapefruit juice can interfere.
- Get a CK blood test. If it’s over 10 times the upper limit, you have myopathy. If it’s 5 times or more, your doctor should consider stopping the statin.
- Temporarily stop the statin. Most muscle symptoms fade within 2-4 weeks. If they do, that’s a strong clue the statin was the cause.
- Switch statins. Try pravastatin 20-40mg. It’s low-risk, cheap, and often just as effective.
- Rechallenge carefully. If symptoms disappeared, your doctor might try a low dose of your original statin again - but only after ruling out interactions.
One study found that 71% of people who thought they were “statin-intolerant” could tolerate a different statin at a lower dose. That’s huge. You’re not broken. You just need the right match.
Alternatives When Statins Don’t Work
If you’ve tried everything - different statins, lower doses, avoiding interactions - and your muscles still hurt, there are options.Bempedoic acid (Nexletol) is the newest. It lowers cholesterol without entering muscle cells. That means no myopathy. But it costs over $4,000 a year. Generic atorvastatin? $6.60. So it’s not a first-line fix.
Icosapent ethyl (Vascepa) is another tool. It’s not a statin - it’s a purified fish oil. It reduces heart attacks in people already on statins. For some, it means they can drop to a lower statin dose - reducing muscle risk while keeping heart protection.
And yes, some doctors suggest coenzyme Q10. The evidence is mixed, but if you’re on a statin and feel drained, it’s low-risk to try 100-200mg daily. No harm, maybe some help.
What Your Doctor Should Be Doing
You shouldn’t have to remember all this. Your doctor should be proactive.- Check your meds list every time you refill a statin.
- Ask about muscle symptoms - not just when you complain, but routinely.
- Order baseline CK before starting, and repeat if symptoms appear.
- Know which statins are safest with your other drugs.
- Never prescribe simvastatin 80mg. It’s been shown to carry 5-10 times the risk of myopathy compared to lower doses.
That last point matters. The European Atherosclerosis Society banned simvastatin 80mg in 2015. The FDA didn’t. But doctors who know better avoid it entirely.
Bottom Line: Statins Are Still Worth It - If You Manage the Risk
Statins prevent heart attacks. They save lives. But they’re not harmless. The key isn’t avoiding them - it’s avoiding the dangerous combinations.If you’re on a statin and taking another medication, ask: “Could this be making my muscles hurt?” If you’re over 70, have kidney issues, or take multiple drugs, get a CK test. If you’re on simvastatin or lovastatin and taking an antibiotic, ask if azithromycin is an option. If you’re on gemfibrozil, ask if fenofibrate will work instead.
There’s no shame in switching statins. There’s no shame in asking for help. And there’s no reason to suffer muscle pain when safer options exist.
Can I take ibuprofen with statins if I have muscle pain?
Yes, ibuprofen and other NSAIDs like naproxen don’t interact with statins in a way that increases myopathy risk. They won’t fix the root cause, but they can help manage pain while you and your doctor figure out if the statin needs to be changed. Avoid long-term use without medical advice, though - NSAIDs carry their own risks for kidneys and stomach.
Does grapefruit juice really affect statins?
Yes - but only with certain ones. Grapefruit blocks CYP3A4, so it can raise levels of simvastatin, lovastatin, and atorvastatin. A single glass won’t cause harm, but daily consumption can build up to dangerous levels. Pravastatin, rosuvastatin, and fluvastatin are safe. If you love grapefruit, switch to one of those.
Can I take CoQ10 supplements to prevent statin muscle pain?
Some people report feeling better on CoQ10, but studies haven’t proven it works consistently. Statins lower CoQ10 levels in the body, so the theory makes sense. Taking 100-200mg daily is safe and low-cost. It won’t fix everything, but it’s worth trying if you’re experiencing muscle fatigue or cramps.
Is it safe to take statins with fish oil supplements?
Yes. Fish oil (omega-3s) doesn’t interfere with statin metabolism. In fact, high-dose prescription fish oil (icosapent ethyl) is often added to statin therapy to further reduce heart risk. Over-the-counter fish oil is fine too - just make sure it’s from a reputable brand with third-party testing.
Why is simvastatin 80mg banned in some countries?
It’s not banned everywhere, but major guidelines (like the European Atherosclerosis Society) recommend avoiding it because the risk of myopathy is 5-10 times higher than with lower doses - with no extra heart benefit. The FDA still allows it, but only for patients who’ve been on it for a year without issues. Most doctors now avoid it entirely.
Can genetic testing tell me if I’m at risk for statin myopathy?
Yes - but it’s not routine. A gene called SLCO1B1 affects how your liver takes up statins. One variant increases simvastatin myopathy risk by 4.5 times. The FDA added this info to simvastatin’s label in 2011. But testing isn’t widely used because it’s expensive and most cases are preventable just by avoiding high-risk combinations. It’s useful if you’ve had unexplained muscle pain on multiple statins.
What Comes Next?
New research is looking at intermittent dosing - like taking rosuvastatin every other day. Early data suggests it keeps cholesterol down while cutting muscle side effects. Results from the DECLARE trial are expected in late 2024. That could change how we prescribe statins for older adults or those with mild muscle symptoms.For now, the message is simple: don’t fear statins. Fear the bad combinations. Talk to your pharmacist. Ask your doctor to review all your meds. And if your muscles hurt - don’t just tough it out. There’s a better way.


Brad Seymour
November 4, 2025 AT 17:14Bro, I was on simvastatin for years and thought I was just getting old. Then my pharmacist flagged the clarithromycin I took for a sinus infection - boom, muscle pain started the next day. Switched to azithromycin and pravastatin, and I’m back to hiking without limping. Don’t ignore your meds list - pharmacists are your real MVPs.
Malia Blom
November 5, 2025 AT 00:49Statins are just Big Pharma’s way of turning healthy people into patients. You think muscle pain is bad? Try living with a liver enzyme profile that looks like a stock market crash. Meanwhile, your doctor’s still pushing ‘low-fat diet’ like it’s 1992. The real villain? Sugar. Not statins. Not interactions. Just stop eating carbs and you won’t need any of this.
Erika Puhan
November 6, 2025 AT 07:30Let’s be clear: the CYP3A4 pathway isn’t some obscure biochemistry footnote - it’s the Achilles’ heel of statin metabolism. When you introduce a CYP3A4 inhibitor like clarithromycin or cyclosporine, you’re essentially disabling the hepatic efflux pump, leading to non-linear pharmacokinetics and supra-therapeutic plasma concentrations. The data is unequivocal. Yet, primary care providers still prescribe simvastatin 80mg like it’s aspirin. This isn’t medicine - it’s negligence.
Edward Weaver
November 6, 2025 AT 14:57U.S. doctors are the only ones who don’t know this stuff. In Europe, they banned simvastatin 80mg because they care about patients. Here? We’re still giving it out like candy. And don’t get me started on grapefruit juice - if you’re drinking that crap with your statin, you deserve the muscle pain. America’s healthcare system is broken because we let people be lazy and dumb.
Lexi Brinkley
November 8, 2025 AT 10:59OMG I just realized my dad’s on simvastatin AND takes grapefruit juice every morning 😱 I’m literally running to his house right now to throw out his juice. 🚫🍊 I’m so glad I read this - thank you for saving lives!! ❤️🩺
Kelsey Veg
November 8, 2025 AT 13:48ok so i was on atorvastatin and started feeling like my legs were made of lead… i thought it was just stress or something. then i found out i was also on diltiazem. duh. switched to pravastatin and boom, energy back. why does no one tell you this stuff??
Alex Harrison
November 10, 2025 AT 04:10Just wanted to add that CoQ10 isn’t a magic fix, but I’ve been taking 200mg daily for six months now and my cramps are way better. I don’t know if it’s placebo or not, but it’s cheap and safe. Also, don’t forget that alcohol makes everything worse - I cut back and noticed a difference even before switching statins. Small changes matter.
Jay Wallace
November 10, 2025 AT 07:16Let’s not pretend this is complicated. If you’re over 70, on multiple meds, and taking simvastatin - you’re playing Russian roulette with your muscles. The FDA’s inaction is criminal. The European guidelines are clear. The science is settled. Yet here we are - in America - where ‘off-label’ means ‘reckless.’ Your doctor isn’t protecting you. They’re just following the script. Wake up.
Alyssa Fisher
November 10, 2025 AT 20:45What’s interesting is how this reflects a deeper flaw in how we treat chronic disease: we optimize for the molecule, not the person. We focus on LDL numbers while ignoring the lived experience of muscle pain, fatigue, and fear. A 78-year-old woman on diltiazem and simvastatin isn’t a ‘risk factor profile’ - she’s someone who just wants to walk her dog without hurting. Maybe the real innovation isn’t a new statin - it’s a system that listens.
Alyssa Salazar
November 11, 2025 AT 01:56Actually, the SLCO1B1 gene variant is underutilized in clinical practice - it’s not just expensive, it’s under-recognized. If you’ve had unexplained myopathy across multiple statins, get tested. It’s a 15-minute blood draw that could prevent years of pain. And yes, intermittent dosing (e.g., rosuvastatin every other day) is emerging as a legit strategy - especially for elderly patients with polypharmacy. The DECLARE trial data will be huge. We’re moving beyond ‘one-size-fits-all’ statin therapy - finally.