More than 10% of people in the U.S. say they’re allergic to penicillin. But here’s the catch: up to 90% of them aren’t. That’s not a typo. Most people who think they’re allergic to penicillin can safely take it again-after proper testing. The same goes for NSAIDs like aspirin and ibuprofen. The problem isn’t always the drug. It’s the label. And that label can cost you more money, expose you to riskier antibiotics, and delay your treatment when you need it most.
What Really Happens in a Drug Allergy?
A true drug allergy is an immune system reaction. Your body sees the drug as a threat and attacks it. That’s different from side effects like nausea or dizziness, which are common but not allergic. Allergic reactions happen fast-usually within an hour. Symptoms include hives, swelling, trouble breathing, low blood pressure, or even anaphylaxis. These are real, dangerous, and need immediate care. Penicillin is the most common culprit. But NSAIDs like aspirin, ibuprofen, and naproxen can trigger reactions too, especially in people with asthma or nasal polyps. These reactions aren’t always IgE-mediated like classic allergies. Sometimes they’re caused by how the drug affects your body’s inflammatory pathways. That’s why NSAID allergies can be trickier to diagnose.Why So Many False Penicillin Allergies?
People get labeled allergic to penicillin for all kinds of reasons. Maybe they had a rash as a kid. Maybe their parent said they were allergic. Maybe they were told to avoid it after a mild reaction that wasn’t even allergic. Skin tests for penicillin look for specific antibodies, but they’re not perfect. One outdated reagent, PPL (Prepared Penicillin Polylysine), gives false positives in up to 70% of cases. That’s why the American Academy of Allergy, Asthma & Immunology says it shouldn’t be used anymore. The gold standard for confirming or ruling out penicillin allergy is a drug challenge. After a negative skin test, doctors give a full dose of amoxicillin under supervision. If no reaction occurs, the allergy label is removed. This simple step can change everything-reducing the need for expensive, broad-spectrum antibiotics like vancomycin or clindamycin. Studies show patients labeled penicillin-allergic cost the healthcare system about $500 more per hospital stay because of these alternatives.Desensitization: How You Can Take a Drug You’re Allergic To
Sometimes, you can’t avoid the drug. Maybe you have a life-threatening infection and penicillin is the only thing that works. Or you need aspirin for heart protection but have an NSAID allergy. That’s where desensitization comes in. Desensitization isn’t a cure. It’s a temporary workaround. You’re not becoming immune. You’re tricking your body into tolerating the drug for one treatment cycle. Once you stop taking it, the tolerance goes away. You’ll need to go through the process again if you need the drug later. The process is controlled and slow. For penicillin and other beta-lactams, a 12-step protocol is common. It starts with a tiny fraction of the full dose-sometimes one ten-thousandth. Every 15 to 20 minutes, the dose doubles. The whole thing takes 4 to 8 hours. Some newer protocols, like the one developed at Brigham and Women’s Hospital, can finish in just over two hours by tripling the dose every 15 minutes. These accelerated methods work for drugs like cefazolin, ceftriaxone, and even paclitaxel (a chemotherapy drug). For NSAIDs like aspirin, the process is different. Instead of a single session, it’s often daily dosing. You start with 30 mg of aspirin and slowly increase: 60 mg, 100 mg, 150 mg, then 325 mg. This can take days or weeks, but once you reach the target dose, you keep taking it daily to stay desensitized. This is common for people with aspirin-exacerbated respiratory disease.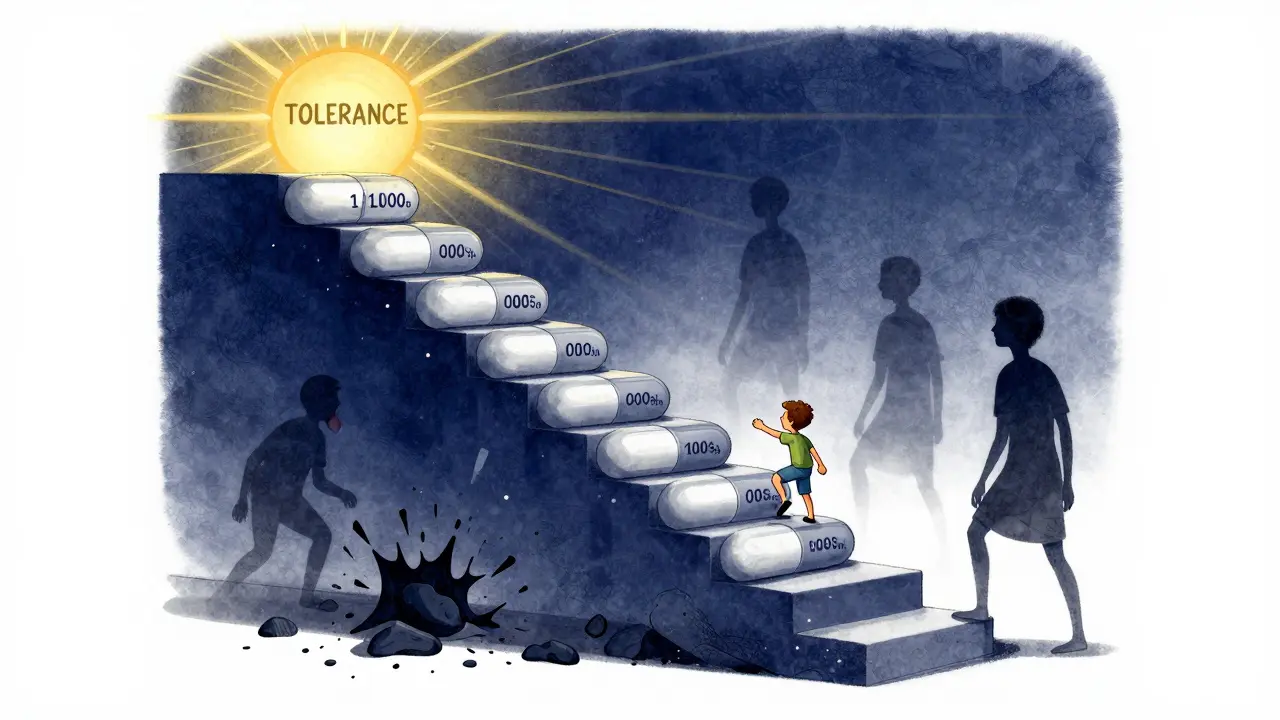
Who Gets Desensitized? And Where?
Desensitization isn’t for everyone. You need two things: a confirmed immediate allergic reaction (like hives, swelling, or anaphylaxis), and no safe alternative. If you can take another antibiotic or painkiller, you should. Desensitization is reserved for when there’s no other option. It’s most often used in hospitals, especially in cancer centers, infectious disease units, and intensive care. Patients with severe infections, cystic fibrosis, or certain cancers rely on it to get life-saving drugs. It’s also used for monoclonal antibodies and chemotherapy agents like carboplatin and rituximab. The procedure must be done by trained staff in a place with emergency equipment on hand. Epinephrine, oxygen, IV fluids, and a team ready to treat anaphylaxis are non-negotiable. If a patient develops severe hypotension or laryngeal edema that doesn’t respond quickly to treatment, the process is stopped.What About Kids?
Most protocols were designed for adults. Children are an afterthought. But kids with allergies to antibiotics or chemotherapy drugs need these options too. The same principles apply: confirm the allergy, rule out alternatives, then proceed with care. Pediatric allergists are working with oncologists and infectious disease specialists to adapt adult protocols for children. The challenge? Kids aren’t just small adults. Their immune systems react differently. Dosing needs to be precise. Monitoring has to be tighter. Right now, there’s no standardized pediatric protocol. That’s a gap in care. Experts agree: we need more research, more guidelines, and more collaboration between specialties to make desensitization safe and accessible for children with chronic diseases or cancer.
The Big Limitation: It’s Temporary
This is the hardest part to accept. Desensitization doesn’t last. It only works during one treatment course. If you need the drug again next month-or next year-you start over. That means repeated hospital visits, more time, more cost, and more risk. Some people worry about becoming re-allergic. Studies show that only about 2% of people who were desensitized to penicillin develop a new reaction when they take it again later. Still, if you had a severe reaction in the past, your doctor might recommend retesting with skin tests before trying desensitization again.What Should You Do If You Think You’re Allergic?
If you’ve been told you’re allergic to penicillin or an NSAID, don’t assume it’s true. Ask your doctor about allergy testing. A simple skin test and oral challenge can clear up decades of unnecessary fear. If you need the drug and can’t avoid it, ask if desensitization is an option. Bring up the possibility. Not every hospital offers it, but major medical centers do. Your allergist, infectious disease specialist, or oncologist can help you find the right team. Don’t let a label from 20 years ago hold you back. You might be able to take the drug safely. You might even save money, avoid side effects from stronger antibiotics, and get better faster.What Happens If You Skip Testing and Just Avoid the Drug?
Avoiding penicillin sounds safe. But it’s not always the right choice. People labeled penicillin-allergic are more likely to get broader-spectrum antibiotics. These drugs kill more good bacteria, increase the risk of C. diff infections, and contribute to antibiotic resistance. They’re also more expensive and sometimes less effective. For NSAIDs, avoiding them might mean using opioids for pain-adding addiction risk. Or using steroids that cause weight gain, mood swings, or bone loss. The trade-offs are real. The bottom line? Don’t live with a label you don’t need. Get tested. Ask questions. Know your options.Can you outgrow a penicillin allergy?
Yes, many people do. Penicillin allergies often fade over time. Studies show that 80% of people who had a reaction as a child lose their sensitivity after 10 years. That’s why it’s important to get retested, especially if you’ve avoided penicillin for decades. A simple skin test and oral challenge can confirm whether you’re still allergic-or if you’re safe to use it again.
Is NSAID desensitization permanent?
No. Unlike penicillin desensitization, which is done in one session, NSAID desensitization often requires daily dosing to maintain tolerance. If you stop taking the drug for more than a few days, your body may lose its tolerance. That means you’ll need to restart the gradual dosing process. This is why it’s mostly used for patients who need daily aspirin for heart protection or those with chronic respiratory conditions.
Can you desensitize to multiple drugs at once?
No. Desensitization protocols are designed for one drug at a time. Trying to desensitize to two drugs together increases the risk of severe reactions and makes it impossible to tell which drug caused a problem. If you need multiple drugs, they’re done separately, with at least a few days between each protocol.
Are there risks with desensitization?
Yes. Desensitization can trigger a reaction-even during the process. That’s why it’s only done in controlled settings with emergency equipment ready. Most reactions are mild: itching, flushing, or nausea. Severe reactions like anaphylaxis are rare but possible. The procedure is stopped immediately if serious symptoms appear. The risk is low when done by experienced teams, but it’s never zero.
Can you do oral desensitization at home?
Never for the initial process. The first time you’re desensitized to a drug, it must be done in a hospital or clinic under supervision. But after successful IV or oral desensitization, some patients can switch to taking the drug orally at home-for example, after being desensitized to an IV antibiotic, they may continue with the oral version. But even then, they’re monitored closely and only after full confirmation of tolerance.
What if I had a reaction years ago but never got tested?
You’re likely not allergic. Most people who report a penicillin allergy from childhood never had a true IgE-mediated reaction. Skin testing and a supervised drug challenge can confirm whether you’re still at risk. Even if you had a rash, hives, or swelling back then, it could have been a viral rash or a non-allergic side effect. Getting tested removes the label and opens up safer, cheaper treatment options.


Mandy Kowitz
January 4, 2026 AT 02:46So let me get this straight - we’re telling people to just *trust* doctors to not mislabel them as allergic after a rash they got at age 7? Cool. I’ll just go ahead and stop wearing seatbelts too, since 90% of car crashes are ‘misdiagnosed’ as deadly.
Also, who wrote this? The pharmaceutical lobby’s intern? Nice spin.
Michael Rudge
January 5, 2026 AT 12:44Oh, the classic ‘penicillin allergy is fake’ narrative. Tell that to the 10% who actually die from anaphylaxis because someone decided to ‘test’ them on a Tuesday afternoon in a clinic with no epinephrine nearby.
And don’t get me started on ‘desensitization’ - it’s just glorified Russian roulette with a white coat. The FDA doesn’t even regulate these protocols properly. You think you’re being saved? You’re just a guinea pig with a clipboard.
Vicki Yuan
January 7, 2026 AT 00:36This is one of the most important public health messages I’ve seen in years. So many people carry around outdated allergy labels like badges of honor - and it’s costing lives, not just money.
My cousin was labeled penicillin-allergic after a rash at 5. At 32, she got tested - turned out she’d outgrown it. She got treated for pneumonia with amoxicillin instead of vancomycin, saved $4,000, and didn’t get C. diff. This isn’t theoretical - it’s life-changing.
Doctors need to stop assuming allergies are permanent. Patients need to ask for testing. And insurance companies need to cover it without 17 forms. Let’s make this standard care, not a luxury.
Jennifer Glass
January 7, 2026 AT 19:39I’ve always wondered why my grandma was told to avoid penicillin after a ‘rash’ that looked like heat rash. She was 8, had chickenpox, and got antibiotics anyway - no reaction. But the label stuck for 60 years.
It makes me think: how many other medical labels are just misunderstandings? Like ‘gluten sensitivity’ or ‘latex allergy’ from a balloon pop.
Maybe we need a national audit of old allergy labels. Not to dismiss real allergies, but to free people from the ghosts of childhood rashes.
Also - desensitization for NSAIDs? That’s wild. I didn’t know you had to keep taking aspirin daily just to stay ‘desensitized.’ Like a drug habit you didn’t ask for.
Joseph Snow
January 8, 2026 AT 10:25Let’s be honest: this entire narrative is manufactured by Big Pharma to push their expensive alternatives. Who benefits from you being ‘allergic’ to penicillin? Not you. Not your doctor. The hospital gets paid more. The pharmacy gets paid more. The lab gets paid for ‘testing.’
And now they want you to pay for a 6-hour ‘desensitization’ protocol? That’s not medicine - it’s a revenue stream.
Don’t be fooled. The real solution? Stop prescribing antibiotics so recklessly in the first place. But that wouldn’t make anyone rich.
John Ross
January 8, 2026 AT 22:50From a clinical pharmacology standpoint, the IgE-mediated vs. non-IgE-mediated distinction in NSAID hypersensitivity is critical - particularly in AERD (aspirin-exacerbated respiratory disease) cohorts. The COX-1 inhibition pathway dysregulation leads to leukotriene overproduction, which is why cross-reactivity is so common among NSAIDs.
Desensitization protocols exploit receptor internalization kinetics and transient T-cell anergy. The Brigham protocol’s accelerated dosing leverages pharmacokinetic saturation thresholds to reduce time-to-tolerance without increasing adverse event incidence - validated in phase II RCTs.
That said, pediatric adaptation remains an unmet need. Current dosing algorithms are extrapolated from adult PK/PD models, which fail to account for ontogenetic differences in CYP450 expression and IgE affinity maturation.
jigisha Patel
January 9, 2026 AT 22:5290% of penicillin allergies are false? That statistic is cherry-picked from a 2015 JAMA study with selection bias. The real figure is closer to 50-60% when you include non-IgE reactions and delayed hypersensitivities.
Also, desensitization has a 12% failure rate in high-risk patients. You’re promoting a procedure that kills people in the name of cost-saving. That’s not medicine - that’s negligence dressed up as innovation.
And why is no one talking about the fact that most of these ‘tests’ are done in academic centers? Rural hospitals can’t afford the staff or equipment. So now you’re creating a two-tiered system: the rich get desensitized, the poor get vancomycin.
Jack Wernet
January 11, 2026 AT 00:06I’ve worked in ICU for 18 years. I’ve seen patients die because they couldn’t get the right antibiotic. I’ve also seen patients have near-fatal reactions because they were mislabeled.
This isn’t about money. It’s about dignity. No one should be forced to suffer through a week of IV antibiotics because a nurse wrote ‘allergic’ on a chart 20 years ago.
I’ve had families cry because they thought their kid couldn’t ever have amoxicillin again. Then we tested them - and they got to go home on a pill. That’s the real win.
Please don’t turn this into a debate about Big Pharma. This is about people. Real people. With real allergies - and real mistakes.
Charlotte N
January 11, 2026 AT 09:47so like… if i had a rash when i was 6 and got told i was allergic… and now i’m 35… and i need penicillin… i should just… go get tested? like… without any fear? what if it’s still there? what if i die? what if they don’t have epinephrine? what if the doctor is busy? what if i’m allergic to the test? what if…
also… why is this so complicated? why can’t we just… know?
Catherine HARDY
January 11, 2026 AT 10:26They say 90% of penicillin allergies are false… but who’s counting? Who’s really tracking this? What if this is just another government-backed lie to make us take more drugs? What if the real reason they want us to get desensitized is so they can slip in GMO antibiotics next? Or maybe they’re testing a new vaccine delivery method? I’ve read things… online… about bioweapons in IV drips…
And why do they always test in hospitals? Why not let us do it at home? Maybe they’re afraid we’ll figure out the truth…
bob bob
January 12, 2026 AT 14:59I love this post. Seriously. I used to be terrified of antibiotics because of a rash I got as a kid. Then I got tested last year - turned out I was fine. Took amoxicillin for a sinus infection. Felt great. Saved $1,200. Didn’t throw up once.
If you’ve been told you’re allergic to something and you’ve never had a real reaction - get checked. It’s not scary. It’s empowering. You’re not weak for being scared. You’re smart for asking.
And if your doctor says ‘no’ - find a new one. This isn’t rocket science. It’s basic medicine.
Uzoamaka Nwankpa
January 12, 2026 AT 23:32Everyone talks about money and tests and protocols… but no one talks about how it feels to be told you’re allergic. To be the person who can’t take a pill. To watch your friends eat painkillers while you sit there with a headache you can’t touch. To be the weird one at the dinner table because you can’t have aspirin.
This isn’t just about antibiotics. It’s about belonging. And if this ‘testing’ doesn’t fix that… what’s the point?
Oluwapelumi Yakubu
January 13, 2026 AT 11:17Man, this whole thing is like being told your soul is cursed because you sneezed near a cat in 1998. You got a label, now you’re branded. Penicillin? NSAIDs? Desensitization? Nah, fam - it’s all just the system trying to reprogram your biology so you stay dependent.
But hey - if you wanna walk into a hospital and let them slowly drip poison into your veins to ‘prove’ you’re not allergic… go ahead. I’ll be over here, sipping turmeric tea and listening to my body.
Truth is, the body remembers. And the body doesn’t lie. Not like the charts do.
Terri Gladden
January 14, 2026 AT 15:06ok so i just read this and i’m crying?? like… i’ve been avoiding penicillin since i was 8 and now i’m 31 and i just found out i might not be allergic?? like… what if i’ve been in pain for years because i was too scared?? what if i could’ve had a simple pill instead of 3 weeks of antibiotics?? what if i’m not broken??
can someone please tell me where to get tested?? i need to know i’m not a liability to my own body
Enrique González
January 14, 2026 AT 23:55Desensitization is a tool. Not a cure. Not a miracle. Just a bridge.
I’ve done it twice - once for cefazolin, once for aspirin. It’s exhausting. It’s expensive. It’s nerve-wracking.
But when you need the drug? It’s the only way. Don’t romanticize it. Don’t fear it. Just understand it.
And if you’re not in a life-or-death situation? Use the alternative. Simple as that.