Decongestant Safety Checker
Decongestant Safety Assessment
This tool helps determine if decongestants (like Sudafed or Afrin) are safe for you based on your heart health. Important: Always consult your doctor before taking any new medication.
Key Risks
Decongestants can raise blood pressure and strain your heart. They're especially dangerous if you have:
- Uncontrolled high blood pressure
- Heart failure
- Arrhythmias
- Prinzmetal angina
- Recent heart attack or stroke
If you’ve got a stuffy nose and a history of heart problems, reaching for that cold medicine might be riskier than you think. Decongestants like pseudoephedrine and phenylephrine are everywhere-on pharmacy shelves, in multi-symptom cold tablets, even in nasal sprays. They work fast. But for people with heart disease or high blood pressure, they can turn a simple cold into something dangerous.
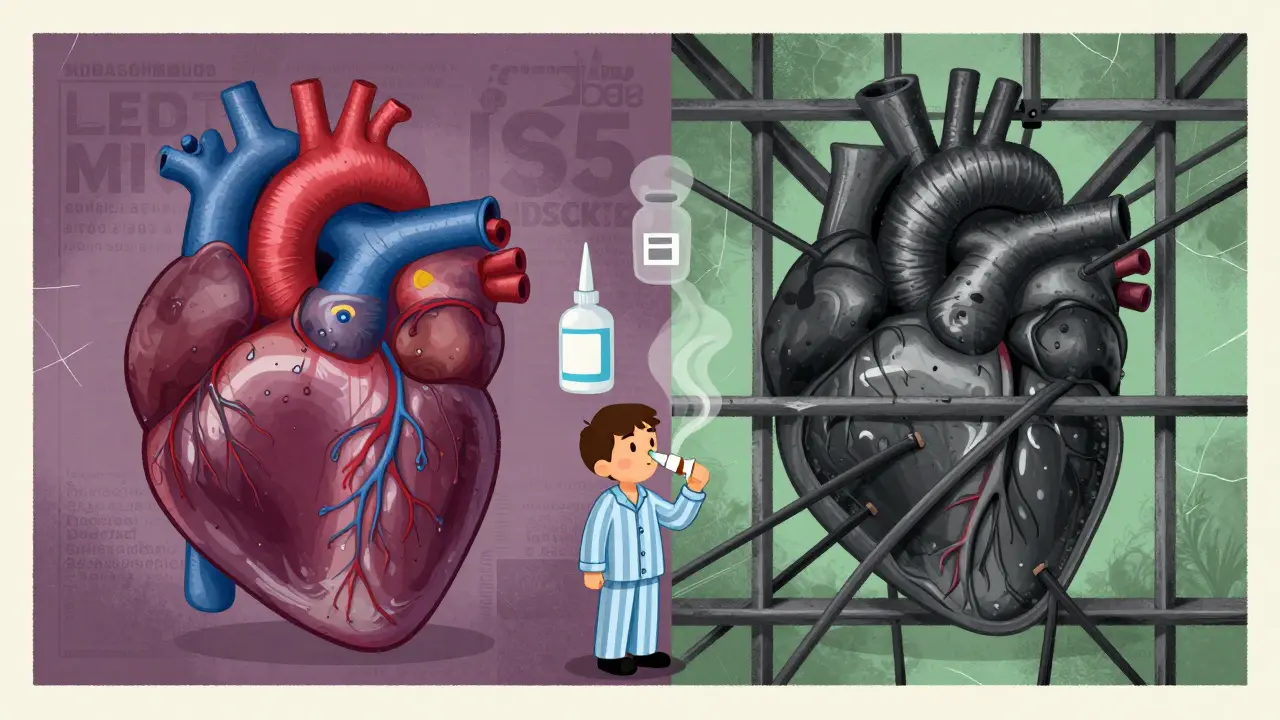
How Decongestants Actually Work
Decongestants shrink swollen blood vessels in your nose to clear congestion. That’s why you feel better within minutes. But here’s the catch: they don’t just target your nose. These drugs are alpha-adrenergic agonists, meaning they trigger the same receptors in blood vessels all over your body. That includes your heart and arteries.
When those receptors activate, your blood vessels tighten. Blood pressure rises. Your heart has to pump harder. For someone with healthy circulation, this might be a minor blip. For someone with heart disease, it’s like revving a worn-out engine.
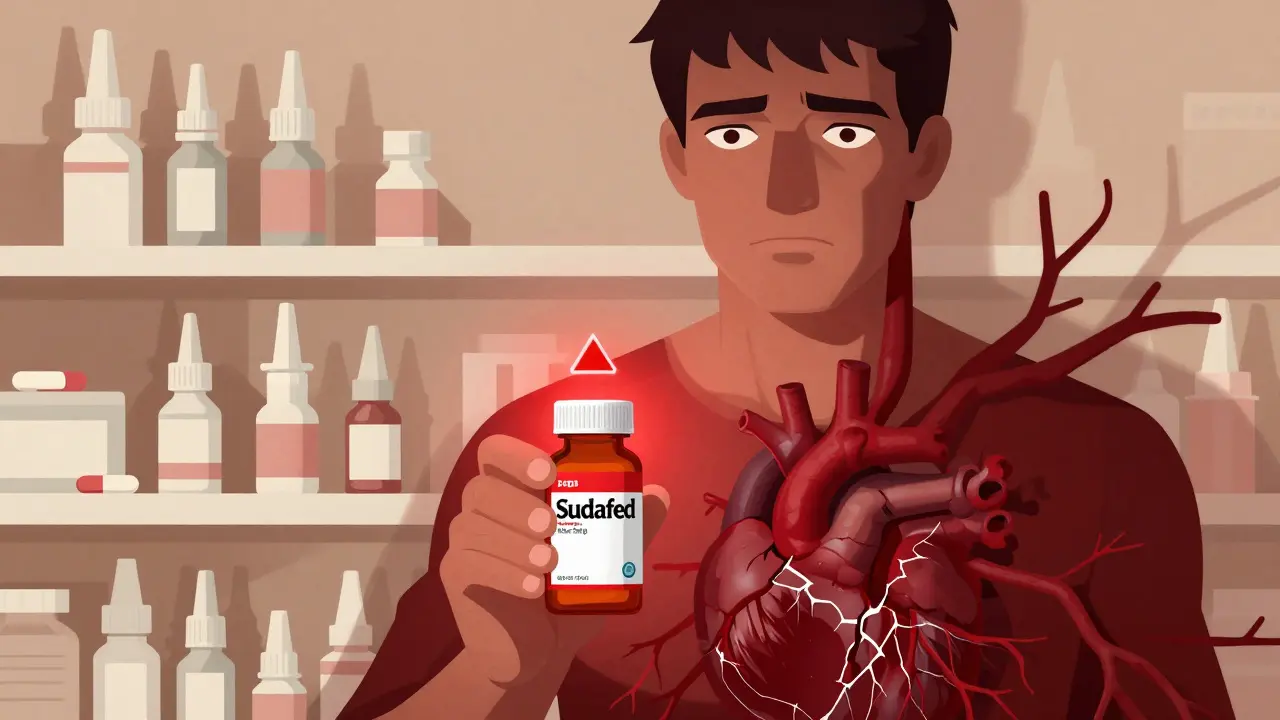
Pseudoephedrine, the active ingredient in Sudafed, has been around since the 1920s. It’s effective. But it’s also been linked to measurable spikes in systolic blood pressure-even in small doses. A 2005 meta-analysis found that even a single dose could raise systolic pressure by 2 to 5 mmHg on average. That might sound small, but for someone with uncontrolled hypertension, that’s enough to push them into danger.
Who’s at Risk?
Not everyone with heart issues needs to avoid decongestants entirely-but some people absolutely should. Medical experts agree on four high-risk groups:
- People with uncontrolled high blood pressure
- Those with heart failure
- Individuals with a history of arrhythmias or irregular heartbeat
- Patients with Prinzmetal angina (coronary artery spasms)
The American Heart Association is blunt: people with uncontrolled hypertension or heart disease should avoid oral decongestants. The same goes for those who’ve had a heart attack or stroke-even if it happened years ago. Your arteries may still be fragile.
Even topical nasal sprays aren’t always safe. Oxymetazoline (Afrin) and naphazoline are meant to act locally, but case reports show they can still cause serious problems. One 40-year-old man developed life-threatening heart failure after overusing a nasal spray containing naphazoline. He didn’t have a prior history of heart disease-but the medication pushed his system past the breaking point.
Why Over-the-Counter Doesn’t Mean Safe
Just because you can buy decongestants without a prescription doesn’t mean they’re harmless. In fact, that’s part of the problem. People assume OTC = safe. But the FDA requires all decongestant packaging to include warnings for high blood pressure and heart disease. If you’re reading the label and skipping over that part, you’re putting yourself at risk.
Pseudoephedrine is kept behind the pharmacy counter in many places, including Australia and the U.S., because pharmacists are trained to screen for contraindications. They’re supposed to ask: Do you have heart disease? Are you on blood pressure meds? Have you had a stroke? But not everyone gets asked. And if you’re buying it online or from a self-service shelf, no one’s checking at all.
Even kids aren’t immune. A documented case involved a 5-year-old girl who developed high blood pressure after being given phenylephrine for a cold. Her blood pressure normalized only after stopping the medication. No other cause was found. That’s not rare-it’s a warning.
What About Alternatives?
You don’t need decongestants to feel better. In fact, for many people with heart conditions, avoiding them is the smartest move.
- Saline nasal sprays are completely safe. They flush out mucus without affecting blood pressure.
- Humidifiers add moisture to the air, helping loosen congestion naturally.
- Guaifenesin (Mucinex) thins mucus without constricting blood vessels. It’s a good option if you’re coughing up phlegm.
- Steam inhalation or a hot shower can open nasal passages without drugs.
- Rest and hydration are still the most powerful tools your body has to fight off colds.
The European Journal of General Medicine puts it plainly: “All these decongestant agents give only symptomatic relief and they don’t treat flu and allergic disease. For this reason, if the symptoms are mild or moderate, not using these agents will be more wisely.” In other words, if your nose is stuffy but you’re not struggling to breathe, let it run its course.
The Hidden Danger: Illness Itself
Here’s something most people don’t realize: just having a cold or the flu stresses your heart. Your body’s fighting an infection. Your heart rate goes up. Inflammation spreads. Blood becomes stickier. All of this increases the chance of a clot or arrhythmia.
A 2017 study of nearly 10,000 heart attack patients found that those who took NSAIDs (like ibuprofen) while sick were more than three times as likely to have another heart attack within a week. Decongestants don’t work the same way, but they add to the same stress. Think of it like piling more weight on a bridge that’s already shaking.
So if you’re sick and have heart disease, you’re not just choosing between two medications. You’re choosing between two risks: the risk of your symptoms worsening, or the risk of triggering a cardiac event.

What Should You Do?
If you have heart disease or high blood pressure, here’s your action plan:
- Check your meds. Look at every cold, flu, or sinus product you own. Read the active ingredients. If it says pseudoephedrine, phenylephrine, ephedrine, or oxymetazoline, put it back.
- Ask your pharmacist. Even if you’re buying something labeled “for high blood pressure,” double-check. Some products sneak in decongestants under the radar.
- Use non-drug options first. Saline spray, steam, rest, fluids. They work slower, but they’re safer.
- Call your doctor. If your congestion is severe or lasts more than a few days, don’t guess. Get professional advice. There may be a safer prescription option.
There’s no magic pill that clears congestion without any risk. But there are plenty of safe ways to manage it-especially if your heart can’t handle the strain.
Final Thought: Symptom Relief Isn’t Worth the Risk
Decongestants give you quick relief. That’s why they’re popular. But if your heart is already working too hard, quick relief isn’t worth the cost. A few extra days of a stuffy nose are better than a trip to the ER.
The goal isn’t to feel perfectly normal while you’re sick. The goal is to stay alive. And for people with heart disease, that means choosing safety over speed.
Can I take pseudoephedrine if my blood pressure is controlled?
Even if your blood pressure is controlled, pseudoephedrine can still cause spikes. Harvard Health says the increase is usually small in controlled cases-but it’s not zero. Some people are more sensitive than others. The safest approach is to avoid it entirely if you have heart disease. Talk to your doctor before using it, even if you think your numbers are fine.
Is phenylephrine safer than pseudoephedrine?
No. While phenylephrine was once thought to be weaker, recent studies show it raises blood pressure just as much as pseudoephedrine in many people. In fact, one case report showed a 5-year-old developed dangerous hypertension from pediatric doses. Both are risky for heart patients. Neither should be used without medical approval.
Can I use nasal sprays if I have heart disease?
Topical sprays like oxymetazoline (Afrin) are often considered safer because they’re local-but they’re not risk-free. A case study showed a man developed life-threatening heart failure after overusing a nasal spray. Even small amounts can enter the bloodstream, especially if used too often or too long. Limit use to 3 days max, and avoid altogether if you have heart failure or uncontrolled hypertension.
What if I accidentally took a decongestant and feel dizzy or have chest pain?
Stop taking the medication immediately. Sit down, stay calm, and check your blood pressure if you have a monitor. If you feel chest pain, shortness of breath, rapid heartbeat, or severe headache, call emergency services. These could be signs of a hypertensive crisis or arrhythmia. Don’t wait to see if it passes.
Are there any decongestants that are safe for heart patients?
There are no decongestants proven safe for people with heart disease. The only safe options are non-decongestant remedies: saline sprays, humidifiers, steam, rest, and fluids. If your symptoms are severe, your doctor may prescribe a safer alternative, like a nasal corticosteroid (e.g., fluticasone), which doesn’t affect blood pressure.

Patty Walters
January 8, 2026 AT 18:25just got off the phone with my cardiologist after almost taking sudafed last week-thank god i checked. they said even if your bp is 'controlled,' these things can still trigger spikes. i now keep a list of safe meds taped to my medicine cabinet. don't be like me and assume 'otc' means 'safe.'
Kiruthiga Udayakumar
January 9, 2026 AT 01:02people are literally dying because they think 'it's just a cold' and grab whatever's on the shelf. i'm not mad, i'm just disappointed. if you have heart disease and you're still using pseudoephedrine, you're not just being careless-you're gambling with your life. and no, 'i only took one pill' doesn't count as responsible.
tali murah
January 10, 2026 AT 03:48Oh wow. A medical article that doesn’t end with ‘consult your doctor.’ How revolutionary. I’m sure the FDA’s 37-page warning label on every decongestant box is just there for aesthetic purposes. 🙄
Also, I love how ‘non-drug options’ are treated like some hippie alternative, when saline spray is literally the only thing that doesn’t turn your heart into a jackhammer. But sure, keep popping pills like they’re Skittles.
Diana Stoyanova
January 10, 2026 AT 06:04Y’all, I’m a nurse and I’ve seen this too many times. Grandpa takes Sudafed for his cold, ends up in the ER with a BP of 210/110. No prior history of issues? Doesn’t matter. The damage is silent until it’s not. I tell my patients: if your nose is stuffy but you’re not choking? Congrats-you’re still breathing. That’s victory. Let your body heal. Hydrate. Rest. Steam. Humidifiers. These aren’t ‘alternative’-they’re the baseline of smart care. You don’t need a pill to feel better. You need patience. And respect for your heart.
Also, if you’re using Afrin for more than 3 days? You’re not treating congestion-you’re creating a chemical dependency that wrecks your nasal passages AND your BP. I’ve seen it. It’s ugly. Don’t be that person.
Phil Kemling
January 11, 2026 AT 13:06It’s interesting how we treat medicine like a vending machine. Push a button, get relief. But the body isn’t a machine-it’s a system. Decongestants don’t just ‘fix’ your nose; they hijack your autonomic nervous system. The same receptors that shrink nasal vessels are the ones that keep your heart from overworking. When you force them to contract everywhere, you’re not just treating a symptom-you’re disrupting homeostasis.
And yet, we call this ‘modern medicine.’ Maybe what we need isn’t more drugs, but more humility. Letting the body do what it’s designed to do-even if it takes a few extra days. The cold will pass. A heart attack won’t.
Gregory Clayton
January 12, 2026 AT 22:26Man, this is why America’s going to hell. You can’t even buy a cold pill without a background check now. Next they’ll make us sign a waiver before we can sneeze. I’m not gonna let some doctor or some article tell me what I can take when I’m sick. I’ve got a heart condition? Fine. I’ve got a will to live too. I’ll take my chances.
Ashley Kronenwetter
January 13, 2026 AT 16:34While I appreciate the thoroughness of this post, I must emphasize that the term ‘safe’ is being used loosely. There is no such thing as a ‘safe’ decongestant for individuals with cardiovascular pathology-only degrees of risk. The suggestion that saline sprays or humidifiers are ‘alternatives’ is misleading. They are not alternatives-they are the standard of care. Anything else is a compromise.
Additionally, the assertion that ‘a few extra days of a stuffy nose’ are preferable to cardiac events is not merely prudent-it is medically indefensible to ignore. The burden of proof lies with the user of decongestants, not the physician.
Lindsey Wellmann
January 14, 2026 AT 05:32OMG I JUST REALIZED I STILL HAVE A BOTTLE OF AFTRIN IN MY BATHROOM FROM LAST WINTER 😱 I’M DELETING IT RIGHT NOW. 🚫💧 Also, I’m gonna buy a humidifier and start drinking 10 gallons of water a day. My heart will thank me. 🫶❤️
Ian Long
January 14, 2026 AT 09:51I get why people reach for decongestants-they work fast, and when you’re sick, you just want to feel normal again. But that’s the trap. We’ve been conditioned to equate relief with recovery. But sometimes, the most powerful thing you can do is wait. Breathe through it. Let your body do its job. The cold doesn’t care if you’re productive. Your heart does.
And honestly? If you’re the type who needs to ‘do something’ when you’re sick, go take a hot shower, put on sweatpants, and watch a dumb movie. That’s healing too. You don’t need a chemical crutch to be a good person. You just need to be kind to yourself.