Excipients Explained: What They Are and Why They Matter in Your Medications
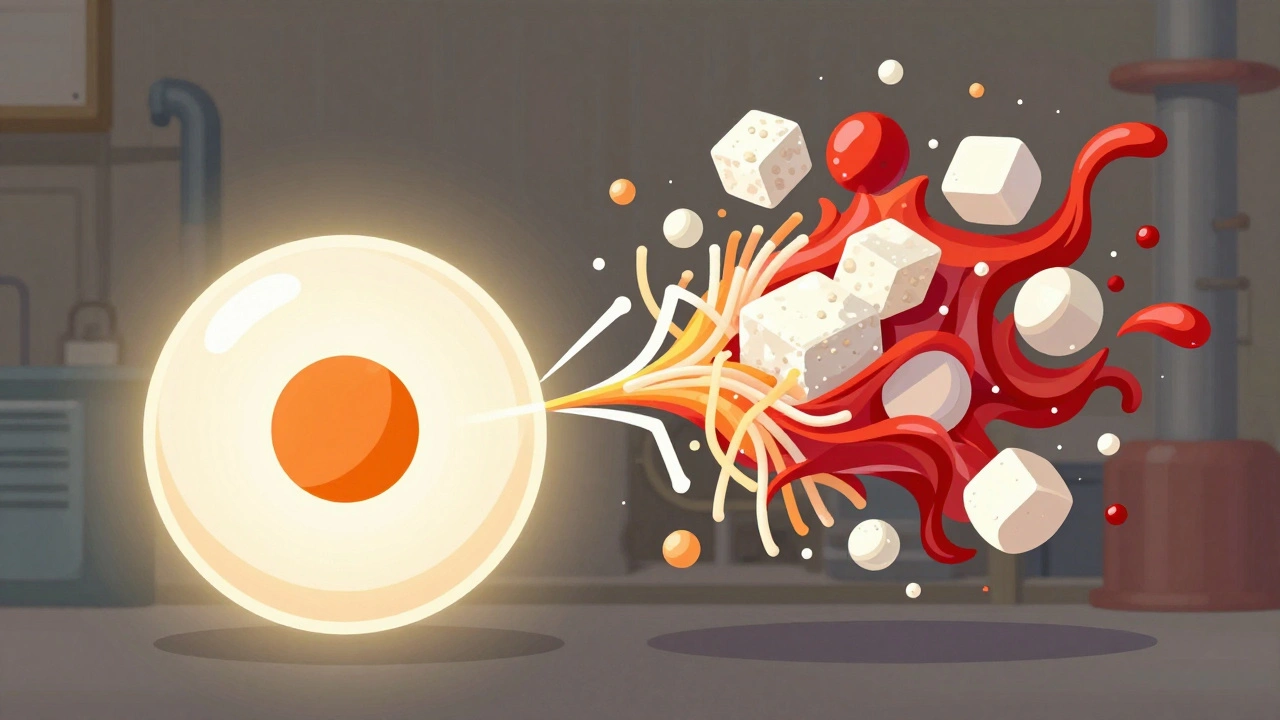
When you take a pill, you’re not just swallowing the active drug. You’re also ingesting excipients, non-active ingredients added to medicines to help with manufacturing, stability, or absorption. Also known as inactive ingredients, these substances make up most of the tablet or capsule — often more than 90% of its weight. They’re not filler in the sense of being useless. Without them, many drugs wouldn’t dissolve properly, would break down too fast, or would be impossible to swallow.
Excipients include things like lactose, cellulose, starch, magnesium stearate, and titanium dioxide. Each has a job: some hold the pill together, others help it break down in your gut, and some even mask bitter tastes. But here’s the catch — not all excipients are safe for everyone. If you’re lactose intolerant, a pill with lactose as an excipient could cause bloating or diarrhea. If you have a corn allergy, the starch in your medication might trigger a reaction. Even colors and coatings can cause problems for people with sensitivities. The FDA requires these ingredients to be listed on the package insert, but most patients never check.
These ingredients also affect how your body absorbs the drug. A tablet designed to release slowly — an extended-release formulation — relies on special excipients to control how fast the active ingredient gets into your bloodstream. Change those excipients, and you might get too much of the drug too fast, or not enough at all. That’s why switching between brand-name and generic versions isn’t always harmless, even when the active ingredient is the same. The drug formulation, the complete recipe of active and inactive ingredients in a medicine matters just as much as the active component.
Manufacturers choose excipients based on cost, stability, and ease of production — not always patient safety. That’s why some people report side effects from a generic version that they never had with the brand-name drug. It’s rarely the active ingredient. It’s the excipients. And because these ingredients aren’t always clearly explained to patients, many assume their reaction is just "in their head." But it’s not. There’s real science behind why one pill makes you feel fine and another gives you a rash or upset stomach.
When you see a post about generic switching, extended-release side effects, or drug-induced liver injury, you’re often looking at the hidden role of excipients. A coating that delays release might cause stomach irritation. A binder made from a specific starch might interfere with absorption in people with gut conditions. Even the lubricants used to push pills through manufacturing machines can trigger allergic reactions in rare cases. These aren’t edge cases — they’re common enough that doctors and pharmacists need to know about them.
Understanding excipients helps you ask better questions. Instead of just asking "Is this generic safe?" you can ask, "What’s in this pill besides the active drug?" You can check if your medication contains gluten, dairy, or artificial dyes. You can spot when a new version of your drug has changed its formulation — and why that might matter for how you feel.
The posts below dive into real cases where excipients played a hidden but critical role — from why some people react to generic warfarin, to how extended-release coatings affect nausea, to why certain medications cause unexpected side effects even when the active ingredient is unchanged. You’ll learn what to look for on the label, how to talk to your pharmacist about ingredients, and when a change in your pill’s appearance might mean more than just a new design.
Inactive Ingredient Differences: Why Your Generic Medication May Feel Different
Generic medications save money but sometimes cause unexpected side effects due to different inactive ingredients. Learn why your body might react differently - and what to do about it.
Read more