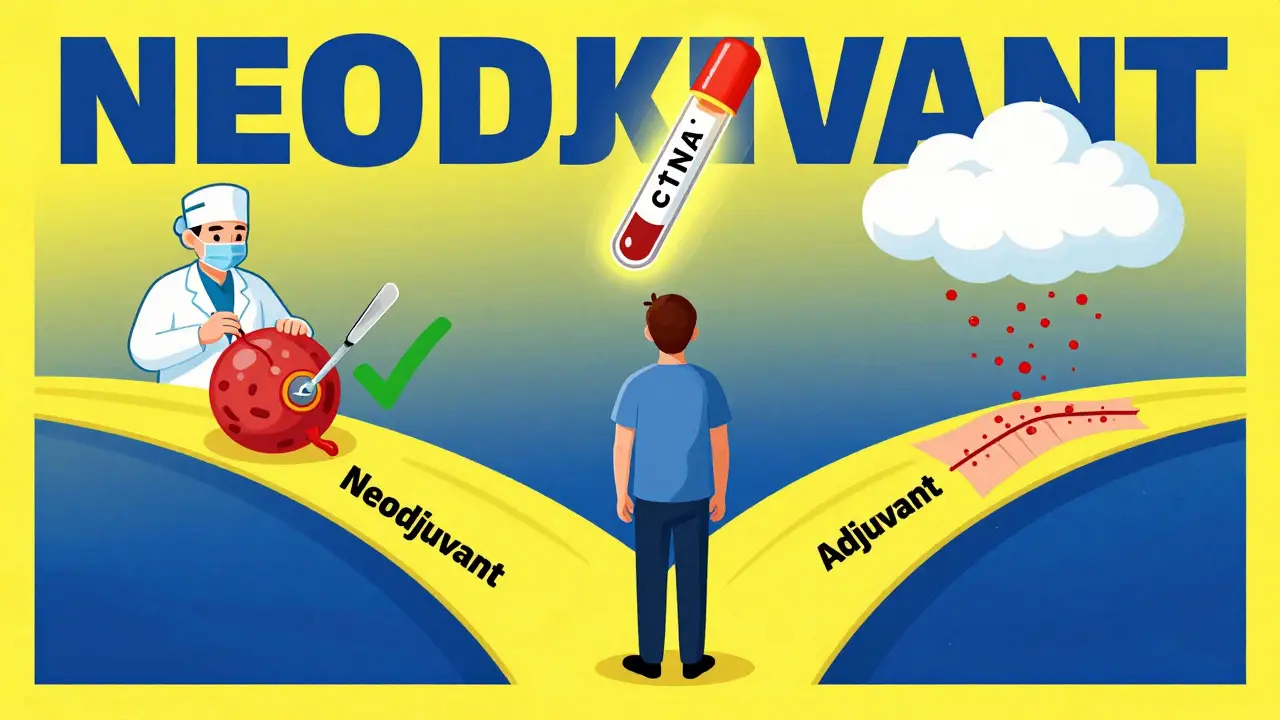
When you’re facing a cancer diagnosis that requires surgery, one of the most important decisions isn’t about the operation itself-it’s about when to give treatment. Should you start chemotherapy or immunotherapy before the surgery to shrink the tumor? Or wait until after, to mop up any leftover cancer cells? This isn’t just a technical question. It’s personal. It affects how long you wait for surgery, how sick you feel, and even your chances of living cancer-free five years from now.
What’s the difference between neoadjuvant and adjuvant therapy?
Neoadjuvant therapy means treatment before surgery. It’s often chemo, immunotherapy, or a mix of both. The goal? Shrink the tumor so it’s easier to remove, kill hidden cancer cells early, and see how your body responds to the drugs while they’re still working inside you. If the tumor shrinks dramatically, that’s a good sign the treatment is working.
Adjuvant therapy comes after surgery. It’s meant to destroy any cancer cells that might have been left behind-cells too small to see on scans, floating in your bloodstream, or hiding in nearby tissue. It’s like cleaning up after the main job is done.
For decades, adjuvant therapy was the standard. Surgery first, then drugs. But in the last 10 years, things have flipped in many cases. Now, for certain cancers-especially lung and breast-doctors are choosing to treat before surgery more often.
Why treat before surgery? The real advantages
One of the biggest reasons doctors prefer neoadjuvant therapy is that it gives you real-time feedback. You don’t have to guess whether the drugs are working. After a few cycles-usually 3 to 4 over 9 to 12 weeks-you go in for surgery. The pathologist examines the removed tissue and tells you exactly how much cancer was killed.
This is called a pathologic complete response, or pCR. It means no live cancer cells are found in the tumor after treatment. In triple-negative breast cancer, patients who achieve pCR have a much better chance of surviving long-term. In non-small cell lung cancer, a 2022 study in The New England Journal of Medicine showed that when patients got neoadjuvant immunotherapy plus chemo, 24% achieved pCR. With chemo alone? Just 2.2%.
Another benefit? Early treatment. Cancer can spread silently before surgery. Neoadjuvant therapy attacks those invisible cells right away. It also reduces the chance that cancer will become resistant to treatment. When you give drugs before surgery, you’re hitting the tumor when it’s still mostly vulnerable.
And then there’s the practical side. Sometimes, the tumor is too big or too close to vital structures to remove safely. Neoadjuvant therapy can shrink it enough to make surgery possible at all. In one study, 15% of patients who started with stage III lung cancer were able to have a less invasive surgery after neoadjuvant treatment.
What about adjuvant therapy? Why still use it?
Adjuvant therapy isn’t outdated. It’s still the go-to for many patients, especially if the cancer is caught early or if neoadjuvant therapy isn’t an option. For some, the idea of waiting weeks for treatment before surgery is too stressful. They want the tumor out as soon as possible.
Also, not all tumors respond well to neoadjuvant treatment. If a patient’s cancer is slow-growing or hormone-sensitive, like some estrogen-receptor-positive breast cancers, doctors may still prefer to remove it first and then use hormone therapy afterward.
And here’s the catch: adjuvant therapy is predictable. You know you’re going to have surgery. You know what’s left behind. You can tailor the drugs to the tumor’s specific biology after it’s removed. That’s harder to do before surgery, when you’re working with limited tissue.
Neoadjuvant + adjuvant: Is more better?
Here’s where things get complicated. In 2022, the FDA approved a combo: neoadjuvant immunotherapy plus chemo, followed by more immunotherapy after surgery. It looked great in the CheckMate 816 trial-patients lived longer without their cancer coming back.
But a major 2024 study in JAMA Network Open looked at four large trials involving over 3,000 patients with lung cancer. The results? Adding adjuvant immunotherapy after neoadjuvant therapy didn’t improve survival. It did, however, increase severe side effects-from 17.6% to nearly 30%.
That’s a big deal. Severe side effects mean hospital stays, missed work, nerve damage, and long-term fatigue. If you’re not getting more life out of it, why risk more harm?
Now, leading experts are questioning whether the post-surgery dose is even necessary. Dr. Mark Awad from Dana-Farber says, “The neoadjuvant-only approach may represent the optimal sequencing strategy.”
In breast cancer, the data is mixed. A 2023 analysis of over 1,000 patients with early-stage triple-negative breast cancer found no big difference in survival between those who got neoadjuvant therapy and those who got adjuvant. But the patients who achieved pCR? They did significantly better-no matter when they got the drugs.
So the real question isn’t “before or after?” It’s “did it work?”
Who gets neoadjuvant therapy? It’s not for everyone
Guidelines from the National Comprehensive Cancer Network (NCCN) recommend neoadjuvant chemoimmunotherapy for patients with stage IB (tumor ≥4 cm) to IIIA non-small cell lung cancer. For breast cancer, it’s standard for triple-negative, HER2-positive, or large hormone-receptor-positive tumors.
But it’s not just about the stage. Your tumor’s biology matters. PD-L1 expression levels help predict if immunotherapy will work. If your tumor has low PD-L1, you might not benefit from immunotherapy at all-neoadjuvant or otherwise.
Also, your overall health. If you have heart problems, lung disease, or other conditions, you might not tolerate the side effects of neoadjuvant treatment. Toxicity can delay surgery by weeks. About 10-15% of patients need to postpone their operation because of side effects like low white blood cell counts or lung inflammation.
And then there’s access. Only 58% of community hospitals in the U.S. have formal neoadjuvant pathways. At academic centers? 92%. That means where you live and where you get care can affect your options.
What’s changing in 2025 and beyond?
The future of treatment sequencing is getting smarter. Instead of treating everyone the same, doctors are starting to use circulating tumor DNA (ctDNA)-tiny pieces of cancer DNA floating in the blood-to guide decisions.
After neoadjuvant therapy and surgery, if ctDNA is still detectable, that’s a red flag. It means cancer cells are still hiding. Those patients are more likely to relapse. In trials like KEYNOTE-867 and NeoADAURA, doctors are now using ctDNA to decide who needs more treatment after surgery-and who doesn’t.
That’s a game-changer. It means you might avoid months of unnecessary chemo if your ctDNA is clean. Or get stronger treatment if it’s not.
Another shift? More personalized timelines. Instead of giving 4 cycles of chemo to everyone, some centers are now testing after 2 cycles. If the tumor isn’t shrinking, they switch drugs before surgery. That’s called adaptive therapy.
By 2030, experts predict 70% of early-stage lung cancer patients will get biomarker-driven neoadjuvant therapy. And survival rates? They could jump from 68% to over 80%.
What should you ask your doctor?
If you’re facing surgery for cancer, here are five questions to ask:
- Is neoadjuvant therapy an option for my type and stage of cancer?
- Will we test for PD-L1 or other biomarkers before deciding?
- What’s the chance I’ll achieve a pathologic complete response?
- If we do neoadjuvant therapy, will you still give more treatment after surgery-and why?
- How will we monitor my response during treatment? Will we use scans, biopsies, or blood tests like ctDNA?
Don’t be afraid to ask for a second opinion. Treatment sequencing is one of the most nuanced decisions in modern oncology. There’s no one-size-fits-all answer. What works for someone else might not be right for you.
The goal isn’t just to remove the tumor. It’s to remove the risk. And sometimes, the best way to do that is to start treating before you even go into the operating room.
Real stories, real choices
A 58-year-old man in Melbourne with stage IIB lung cancer chose neoadjuvant nivolumab and chemo. After three cycles, his tumor shrank by 90%. His surgeon said he’d have been able to do a wedge resection instead of a full lung removal. He got no adjuvant therapy. Two years later, he’s cancer-free.
A 47-year-old woman with triple-negative breast cancer opted for adjuvant chemo because she was terrified of waiting. Later, she learned her tumor had a high risk of recurrence. She wishes she’d known that neoadjuvant therapy could have given her a clearer picture of her prognosis.
There’s no perfect choice. But the more you know about your options, the better your decision will be.

Jenci Spradlin
January 8, 2026 AT 04:17man i just had my bro go through this last year for stage 3 lung cancer. neoadjuvant was the way to go - tumor shrunk so bad they did a lobe removal instead of the whole lung. no adjuvant needed. doc said his pCR was crazy good. i didn’t even know what that word meant till i looked it up. now i’m the family expert lol.
Heather Wilson
January 8, 2026 AT 20:23While I appreciate the attempt at simplifying a complex oncological paradigm, the article fundamentally misunderstands the hierarchical nature of evidence-based sequencing. The reliance on pCR as a surrogate endpoint is statistically dubious when not validated against overall survival in prospective, randomized, phase III trials with adequate power. The JAMA Network Open meta-analysis you cite explicitly demonstrates no OS benefit with dual-phase therapy - a finding that should supersede anecdotal success stories and institutional bias toward aggressive interventionism. Furthermore, the normalization of ctDNA monitoring as a decision-making tool lacks FDA approval for this specific indication, rendering its clinical utility speculative at best.
Chris Kauwe
January 8, 2026 AT 21:04Let’s be real - this whole neoadjuvant vs. adjuvant debate is just another symptom of Western medicine’s obsession with interventionist dogma. The body isn’t a machine to be fixed with chemicals and scalpels. It’s an ecosystem. You don’t bombard it with immunotherapy like it’s a warzone - you restore balance. The fact that we’re even debating whether to poison patients before surgery speaks to a deeper spiritual decay in healthcare. What happened to watchful waiting? To holistic healing? To trusting the body’s innate intelligence? We’ve replaced wisdom with algorithms and biomarkers.
Meghan Hammack
January 10, 2026 AT 08:37OH MY GOSH. I just read this and cried. My sister had triple-negative breast cancer and they did neoadjuvant chemo first - she got pCR and now she’s hiking in Colorado with her kids. But the side effects? Ugh. She lost her hair, couldn’t walk up stairs, and cried every night. But she said it was worth it. If you’re scared? You’re not alone. But please, please ask for that ctDNA test. It could save you from more chemo you don’t need. You got this.
RAJAT KD
January 11, 2026 AT 14:11Neoadjuvant therapy is not universally superior. In India, access to biomarker testing is limited to 12% of centers. Many patients receive adjuvant therapy not because it’s preferred, but because it’s the only option available. The article ignores global inequity. Survival data from Western trials cannot be extrapolated to resource-limited settings without context.
Matthew Maxwell
January 11, 2026 AT 23:40It is both irresponsible and morally negligent to promote neoadjuvant therapy as a default strategy without first ensuring that patients possess the cognitive capacity to comprehend the risks of delayed surgery, the likelihood of treatment-related complications, and the statistical probability of achieving a pathologic complete response. The casual tone of this article normalizes medical decision-making as a lottery - a dangerous precedent. If you are not consulting with a board-certified oncologist who has reviewed your molecular profile in a high-volume center, you are gambling with your life.
Ian Long
January 12, 2026 AT 22:35Heather, I get where you’re coming from - evidence matters. But Chris, you’re missing the point too. This isn’t about philosophy or dogma. It’s about real people. My mom had stage IIB lung cancer. They did neoadjuvant, she got pCR, and now she’s gardening. The science is evolving. We don’t have to pick one side. We can use biomarkers, ctDNA, adaptive dosing - all of it - to make it personal. The goal isn’t to be right. It’s to be right for *them*.
Pooja Kumari
January 14, 2026 AT 00:55I just read this whole thing and I’m so emotional. I mean, like, deep in my soul emotional. I had cancer too, you know? Not the same kind, but the fear? The waiting? The feeling that your body is betraying you? It’s all the same. And when they said ‘we’re going to start chemo before surgery’ - I screamed. I cried. I didn’t sleep for three nights. But now I’m five years out and I think about that decision every single day. I wish I’d known about ctDNA. I wish someone had told me it was okay to be scared. And I wish I hadn’t felt so alone. You’re not alone. I’m here. I’m typing this. You’re not alone.