Letrozole is one of the most effective and widely used drugs to help women ovulate when they’re struggling to conceive. Unlike older fertility drugs, it’s not designed as a hormone replacement - it works by gently blocking estrogen production, which tricks the body into making more of the hormones that trigger ovulation. It’s now the first-line treatment for many women with polycystic ovary syndrome (PCOS), and it’s increasingly used even when no clear cause of infertility is found.
How Letrozole Actually Works
Letrozole is an aromatase inhibitor. That sounds complicated, but here’s what it means in plain terms: your body makes estrogen from testosterone and other hormones using an enzyme called aromatase. Letrozole blocks that enzyme. When estrogen levels drop - even just a little - your brain thinks you’re not making enough. So it sends out more follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary gland. Those hormones tell your ovaries to grow and release an egg.
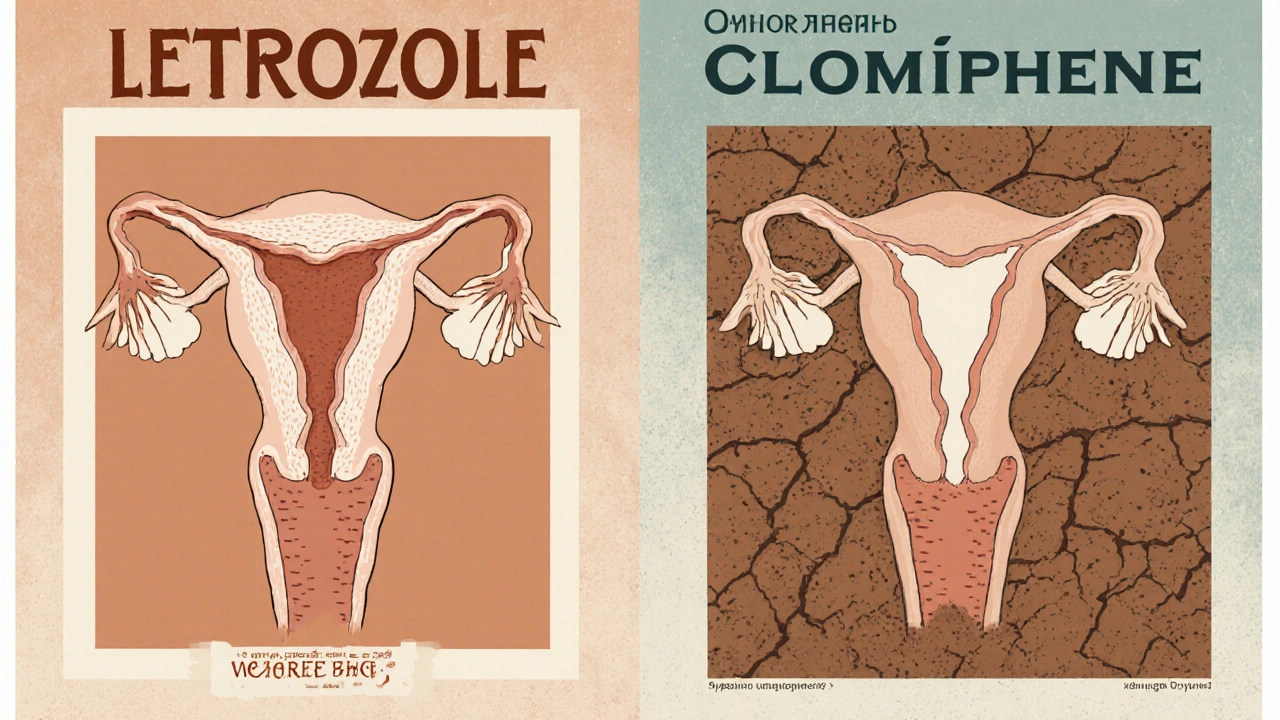
This is different from clomiphene citrate, the older drug used for ovulation induction. Clomiphene works by blocking estrogen receptors in the brain, which also tricks the brain into releasing more FSH. But clomiphene can stick around in your system for weeks and may thin the uterine lining or reduce cervical mucus - problems that can make it harder for sperm to reach the egg. Letrozole clears out of your system in about five days, so it doesn’t interfere with the uterine environment the way clomiphene sometimes does.
Why Letrozole Is Now the First Choice for PCOS
Women with PCOS often have high levels of androgens and insulin resistance, which mess with normal ovulation. For decades, clomiphene was the go-to treatment. But multiple large studies - including the landmark 2014 NIH trial involving over 3,000 women - showed that letrozole leads to higher live birth rates in women with PCOS.
In that study, women taking letrozole had a 27.5% live birth rate after six cycles, compared to 19.1% for those on clomiphene. The difference wasn’t just small - it was meaningful. Letrozole also led to more single pregnancies, which lowers the risk of twins and complications during pregnancy.
Because of this, major guidelines from the American Society for Reproductive Medicine (ASRM) and the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) now recommend letrozole as the first option for ovulation induction in women with PCOS.
Who Can Take Letrozole and Who Should Avoid It
Letrozole is typically prescribed for women who:
- Have irregular or absent periods due to anovulation
- Have been diagnosed with PCOS
- Have unexplained infertility
- Have failed to ovulate with clomiphene
It’s not for everyone. You should not take letrozole if:
- You’re already pregnant - it’s not safe during pregnancy
- You have liver disease - your body needs healthy liver function to process it
- You’re taking estrogen-containing medications - they counteract its effect
- You have a history of blood clots or severe osteoporosis - though this is rare, letrozole can slightly lower bone density with long-term use
It’s also not approved for use in men or for breast cancer prevention outside of oncology settings. Even though it’s used off-label for fertility, it’s still a prescription drug with specific guidelines.
Typical Dosing and Treatment Cycle
Most doctors start with a 2.5 mg daily dose of letrozole. You take it for five days, starting on day 2 to day 5 of your menstrual cycle. If you don’t have regular periods, your doctor might give you a progesterone pill first to trigger a period, then start letrozole on day 2 after that.
Some women respond better to a 5 mg dose, especially if they have higher body weight or didn’t respond to 2.5 mg. Your doctor will monitor you with blood tests and ultrasounds around day 10-12 to check if a follicle has grown to 18-20 mm - the size that usually means ovulation is near.
If ovulation happens, you’ll be advised to have sex every other day for the next few days, or you might get a trigger shot (hCG) to time ovulation precisely. If you don’t ovulate after the first cycle, your dose might be increased to 5 mg or 7.5 mg in the next cycle. Most women who will respond to letrozole do so within three to six cycles.
Side Effects and What to Expect
Letrozole is generally well-tolerated. Most women report mild side effects, if any. Common ones include:
- Hot flashes
- Fatigue
- Headaches
- Mild bloating or abdominal discomfort
- Mood swings or irritability
These usually go away after you stop taking it. Unlike clomiphene, letrozole doesn’t commonly cause visual disturbances or thickened uterine lining. You’re less likely to have multiple pregnancies with letrozole - the twin rate is about 5-8%, compared to 8-10% with clomiphene. Triplets are very rare.
Some women worry about birth defects. Large studies tracking thousands of babies born after letrozole use show no increase in major congenital anomalies compared to the general population or to babies conceived after clomiphene use. The data is reassuring.
Letrozole vs Clomiphene: The Real Difference
Many women are told to try clomiphene first because it’s cheaper and older. But the evidence now clearly favors letrozole for most women, especially those with PCOS.
| Feature | Letrozole | Clomiphene Citrate |
|---|---|---|
| Typical dose | 2.5-7.5 mg daily for 5 days | 50-150 mg daily for 5 days |
| Half-life in body | ~2 days | ~5-7 days |
| Live birth rate (PCOS) | 27-30% | 19-22% |
| Twin pregnancy rate | 5-8% | 8-10% |
| Effect on uterine lining | Neutral or slightly improved | Often thinner |
| Effect on cervical mucus | Minimal impact | Often dries it up |
| Cost (Australia, 2025) | $15-$30 per cycle | $10-$20 per cycle |
While clomiphene is cheaper, letrozole often works faster and with better outcomes. Many fertility clinics in Australia now start with letrozole unless there’s a specific reason not to.

What Happens If Letrozole Doesn’t Work?
If you’ve tried three to six cycles of letrozole and haven’t ovulated or conceived, your doctor will likely move to the next step. That could mean:
- Adding metformin if you have insulin resistance (common in PCOS)
- Switching to injectable gonadotropins (FSH/LH shots)
- Considering laparoscopic ovarian drilling (a minor surgery that can restore ovulation)
- Moving to IVF if you’re over 35 or have other fertility factors
It’s important to remember that fertility treatment is often a process of trial and adjustment. Not every woman responds the same way, and that’s normal.
Where to Get Letrozole and What to Watch For
Letrozole is available by prescription only. In Australia, it’s listed on the Pharmaceutical Benefits Scheme (PBS) for breast cancer treatment, but not yet for fertility. That means you’ll pay the full retail price - around $15 to $30 per cycle, depending on the pharmacy. Some private health insurers may offer partial rebates under extras cover if you have fertility-related benefits.
Never buy letrozole online from unverified sellers. Counterfeit versions are common, and they may contain wrong doses or harmful fillers. Always get it from a licensed pharmacy with a prescription from a qualified fertility specialist or gynaecologist.
When to See a Fertility Specialist
You don’t need to wait a full year to get help. If you’re under 35 and have been trying for 12 months without success, or if you’re over 35 and trying for 6 months, it’s time to see a specialist. If you have PCOS, irregular periods, or a history of miscarriage, you should seek help even sooner.
A fertility specialist will check your hormone levels, do an ultrasound to look at your ovaries, and possibly test your partner’s sperm. From there, they’ll decide if letrozole is right for you - or if another path is better.
There’s no shame in needing help. One in six couples in Australia face fertility challenges. And for many, letrozole is the turning point that leads to a healthy pregnancy.
Is letrozole safe for long-term use in fertility treatment?
Letrozole is only used for short cycles - usually five days per month - during fertility treatment. There’s no evidence that short-term use harms long-term health. It doesn’t build up in your system, and studies tracking women for years after use show no increased risk of cancer, heart disease, or osteoporosis. It’s not meant for continuous daily use like hormone replacement therapy.
Can you take letrozole without having a period?
Yes. If you haven’t had a period in months, your doctor may give you a course of progesterone (like medroxyprogesterone) to induce a withdrawal bleed. Once that happens, you start letrozole on day 2 of your new cycle. This resets your hormonal clock so the drug can work properly.
Does letrozole cause weight gain?
Weight gain isn’t a common side effect of letrozole. Some women report feeling bloated during treatment, but that’s usually temporary and tied to ovulation, not the drug itself. In fact, for women with PCOS, letrozole often helps improve insulin sensitivity, which can make it easier to manage weight over time.
How soon after stopping letrozole does ovulation happen?
Ovulation typically occurs 5 to 10 days after the last dose of letrozole. That’s why doctors schedule ultrasounds around day 10-12 of your cycle. If the follicle is mature, they may give a trigger shot (hCG) to time ovulation within 36 hours.
Is letrozole better than Clomid for unexplained infertility?
For unexplained infertility, letrozole is often preferred because it doesn’t negatively affect cervical mucus or the uterine lining like Clomid can. Studies show similar pregnancy rates, but letrozole has fewer side effects and a lower chance of multiples. Many specialists now start with letrozole even when no clear cause of infertility is found.


Leonard Buttons
October 31, 2025 AT 03:40Alice Minium
October 31, 2025 AT 05:57Adrian Clark
October 31, 2025 AT 20:56Rob Giuffria
November 2, 2025 AT 18:55Barnabas Lautenschlage
November 3, 2025 AT 12:40Ryan Argante
November 5, 2025 AT 10:36Jeanette Case
November 5, 2025 AT 13:50Stephen Maweu
November 6, 2025 AT 02:42anil kharat
November 7, 2025 AT 13:50Keith Terrazas
November 7, 2025 AT 14:01Matt Gonzales
November 9, 2025 AT 05:12Richard Poineau
November 9, 2025 AT 08:17Angie Romera
November 10, 2025 AT 04:28Julisa Theodore
November 10, 2025 AT 10:51Lenard Trevino
November 11, 2025 AT 03:28