Every parent has been there: your child is sick, feverish, cranky, and you just want them to feel better-fast. So when the doctor mentions antibiotics, it’s tempting to say yes. But here’s the truth: antibiotics don’t work for most childhood illnesses. Giving them when they’re not needed doesn’t help your child-it hurts everyone.
What Antibiotics Actually Do (and Don’t Do)
Antibiotics are powerful drugs designed to kill bacteria or stop them from multiplying. They don’t touch viruses. That means if your child has a cold, the flu, most sore throats, or stomach bugs with vomiting and diarrhea, antibiotics won’t help. In fact, they’ll likely make things worse.Here’s the hard number: 99% of cases with diarrhea and vomiting in kids are caused by viruses. Same with most coughs, runny noses, and ear infections. Only about 20% of sore throats are bacterial-strep throat-and even then, you need a test to know for sure. The rest? Viral. Antibiotics on a virus are like using a hammer to fix a leaky faucet. It doesn’t work, and you end up making a mess.
Doctors don’t prescribe antibiotics lightly anymore. Thanks to years of overuse, bacteria have learned to fight back. Today, nearly half of the common ear infection bugs are resistant to penicillin. That means a drug that used to work perfectly might not work at all now. And that’s not just a problem for your child-it’s a global crisis.
When Antibiotics Are Actually Needed
There are times when antibiotics are necessary-and life-saving. The key is knowing the difference between a virus and a true bacterial infection. Here’s what doctors look for:- Strep throat: A rapid test or throat culture must be positive. Symptoms alone (sore throat, fever) aren’t enough-too many viruses mimic strep.
- Ear infections (acute otitis media): Only if there’s moderate to severe ear pain, fever, or fluid draining from the ear, AND the eardrum looks swollen and red.
- Bacterial sinus infections: If symptoms last more than 10 days without improvement, or if your child gets worse after seeming to get better.
- Pneumonia: Only if tests show bacterial cause (about 10% of cases). Most childhood pneumonia is viral.
- Whooping cough: Confirmed by lab test. Antibiotics can reduce spread if given early.
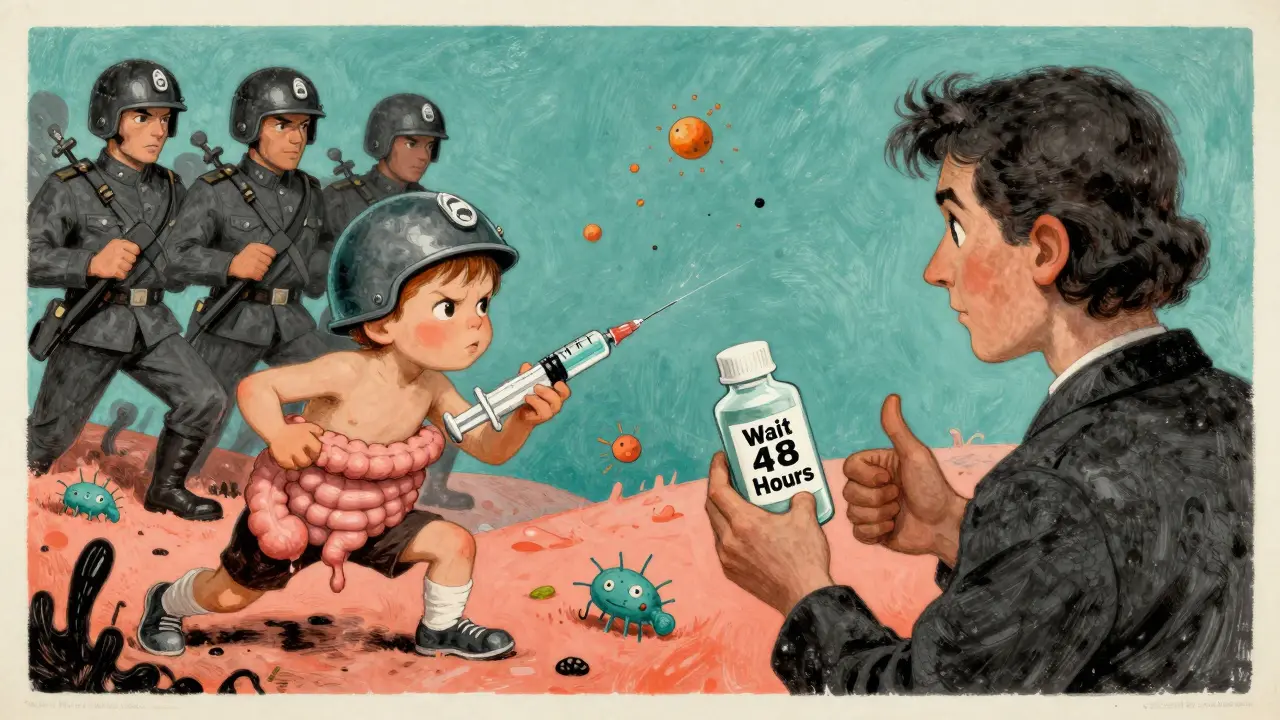
For many cases-like mild ear infections in kids over 6 months-doctors now recommend watchful waiting. Give it 48 to 72 hours. If the child isn’t getting worse, and pain is manageable with ibuprofen, hold off. Often, the immune system clears it on its own.
Common Side Effects in Kids
Even when antibiotics are used correctly, side effects are common. About 1 in 10 children will have some kind of reaction. Most aren’t serious, but they’re annoying-and sometimes scary.- Diarrhea: Happens in 5-25% of kids. It’s usually mild, but can be caused by a dangerous bug called Clostridium difficile if it’s severe or lasts more than a few days.
- Nausea and vomiting: Affects up to 18% of kids, especially with strong-tasting liquids.
- Rash: About 5-10% of children get a rash. Most are harmless-just red spots that fade. But if it’s raised, itchy, or spreads fast, it could be an allergy.
- Yeast infections: Especially in girls, antibiotics can wipe out good bacteria and let yeast grow. Look for diaper rash that won’t go away with zinc oxide, or white patches in the mouth.
Don’t assume every rash is an allergy. Studies show 80-90% of rashes from antibiotics are side effects, not true allergies. That’s why so many kids are wrongly labeled “allergic to penicillin” when they’re not.
True Allergies: When to Worry
A true antibiotic allergy is rare-but dangerous. It’s not just a rash. It’s your child’s immune system going into overdrive. Signs include:- Hives (raised, itchy welts)
- Swelling of the lips, tongue, or face
- Wheezing or trouble breathing
- Vomiting, dizziness, or passing out
If any of these happen, stop the medicine and call emergency services immediately. Anaphylaxis is rare-under 0.05% of antibiotic courses-but it can be fatal if not treated fast.
Here’s something most parents don’t know: if you’re allergic to penicillin, your child isn’t automatically allergic. In fact, 95% of kids labeled allergic because of family history can safely take penicillin. Allergy testing can clear this up. Don’t let a family label stop your child from using a safe, effective drug.

Why Stopping Early Is a Big Mistake
You see your child’s fever gone. Their ear doesn’t hurt anymore. So you stop the antibiotics. Tempting, right? But here’s why that’s dangerous.Antibiotics don’t kill all the bacteria on day two. They kill the weakest ones first. The toughest, smartest bugs survive. If you stop early, those survivors multiply. They become resistant. Next time, the same antibiotic won’t work-and maybe none will.
Studies show 30% of parents stop antibiotics early. That’s one in three kids contributing to the global rise of superbugs. Always finish the full course-even if your child feels better after day two or three.
How to Get Kids to Take Their Medicine
Let’s be honest: most liquid antibiotics taste awful. One study found 43% of kids refuse to take them. Here’s what actually works:- Use a dosing syringe-not a spoon. It’s more accurate and easier to get past the tongue.
- Mix with a small spoonful of chocolate syrup, apple sauce, or juice. Don’t mix with a whole meal-it can affect absorption.
- Ask your pharmacist about flavoring services. Many pharmacies can make amoxicillin taste like bubblegum or strawberry.
- For older kids, capsules can sometimes be opened and mixed into food (check with your doctor first).
If your child vomits within 30 minutes of taking the dose, give the full dose again. If it’s between 30 and 60 minutes, give half. After an hour? No need to repeat-it’s probably absorbed.
The Bigger Picture: Antibiotic Resistance
Every time we give an antibiotic when it’s not needed, we’re playing Russian roulette with future health. The CDC says 30% of antibiotic prescriptions for kids are unnecessary. That’s millions of doses a year that do nothing but fuel resistance.Here’s what’s happening:
- 47% of strep pneumoniae (a common ear and lung bug) are now resistant to penicillin.
- MRSA infections in kids have jumped 150% since 2010.
- Antibiotic-resistant infections cause over 35,000 deaths in the U.S. every year.
- It costs the U.S. healthcare system $4.6 billion annually-just for treating complications from misuse.
This isn’t science fiction. It’s happening now. And it’s being driven by well-meaning parents who think antibiotics fix everything.
What You Can Do
You’re not powerless. You’re actually the most important part of the solution.- Ask: “Is this definitely bacterial?” Don’t accept “It might help” as an answer.
- Ask: “Can we wait 48 hours and see?” For ear infections, sinus issues, or mild pneumonia, watchful waiting is now standard.
- Don’t use leftover antibiotics from another illness. They’re not the same drug, and they might be expired.
- Never pressure your doctor for antibiotics. Studies show 68% of parents feel pressure to ask-even when they know it’s not needed.
- Know that fever doesn’t mean bacteria. Most viral illnesses last 7-10 days. Antibiotics won’t shorten that.
The most powerful tool we have for most childhood illnesses isn’t a drug. It’s time. Rest. Fluids. Ibuprofen. And patience.
What’s Changing Now
Doctors aren’t waiting around. New tools are making smarter decisions possible:- CRP blood tests: These can tell if an infection is bacterial or viral in minutes. Clinics using them have cut unnecessary antibiotics by 85%.
- Rapid susceptibility tests: The FDA approved one in early 2023 that gives results in 6 hours-not 3 days. That means doctors can pick the right antibiotic faster, avoiding broad-spectrum drugs.
- Procalcitonin-guided therapy: A blood marker that rises only with serious bacterial infections. Used in research, it cut unnecessary antibiotic use by 62%.
These aren’t futuristic ideas. They’re in use now-and they’re changing how kids are treated.
Can antibiotics make my child’s diarrhea worse?
Yes. Antibiotics kill good bacteria in the gut, which can lead to diarrhea. In most cases, it’s mild and goes away after stopping the medicine. But if the diarrhea is severe, watery, bloody, or lasts more than a few days, it could be a dangerous infection called C. diff. Call your doctor right away if this happens.
My child had a rash after antibiotics. Does that mean they’re allergic?
Not necessarily. Most rashes from antibiotics (80-90%) are side effects, not allergies. A true allergy includes hives, swelling, trouble breathing, or vomiting. A flat, pink, itchy rash is usually harmless. But if you’re unsure, talk to your doctor. Never assume your child is allergic based on a single rash-many kids are mislabeled.
Is it safe to give my child leftover antibiotics from a previous illness?
No. Antibiotics are prescribed for specific infections, at specific doses. What worked for an ear infection last month won’t help a sore throat now. The wrong drug can delay real treatment, cause side effects, or make bacteria resistant. Always get a new prescription.
Why do doctors wait 48 hours before prescribing antibiotics for ear infections?
Most ear infections in children are viral and clear up on their own within 2-3 days. Giving antibiotics right away doesn’t speed up recovery-it just increases side effects and resistance risk. Waiting 48 hours gives the body a chance to heal naturally. If symptoms get worse or don’t improve, then antibiotics are added.
Can antibiotics cause yeast infections in girls?
Yes. Antibiotics kill good bacteria that normally keep yeast in check. This can lead to a yeast infection in the diaper area or mouth (thrush). Signs include a bright red, patchy rash that doesn’t improve with diaper cream, or white patches in the mouth. It’s treatable with antifungal creams or drops. Talk to your doctor if you suspect it.
My child is allergic to penicillin-does that mean they can’t take any antibiotics?
No. Many kids labeled penicillin-allergic aren’t truly allergic. In fact, 95% can safely take it after proper testing. Other antibiotics like cephalosporins or macrolides are often used instead, but they’re not always the best choice. Ask about allergy testing-it can open up safer, more effective treatment options.
What to Do If Your Child Isn’t Getting Better
If your child is on antibiotics and doesn’t improve after 48-72 hours, call your doctor. Don’t just keep giving it. That could mean:- The infection isn’t bacterial-antibiotics won’t help.
- The bacteria are resistant to the drug.
- There’s a complication you didn’t know about.
Your doctor might need to switch antibiotics, run more tests, or consider a different diagnosis entirely. Don’t wait. Early action stops small problems from becoming big ones.
Antibiotics are miracles-when used right. But they’re not magic. The best thing you can do for your child isn’t rushing to the pharmacy. It’s asking the right questions, trusting the process, and giving your child’s body the time it needs to heal.


Linda Caldwell
December 17, 2025 AT 08:25Just want to say thank you for this. My kid had a bad ear infection last winter and we waited 48 hours like you said. He was grumpy but okay. By day three he was back to drawing dinosaurs and eating pancakes. No antibiotics needed. Trust the process.
Anna Giakoumakatou
December 18, 2025 AT 10:44Oh, how delightful. Another feel-good pamphlet from the American Medical Industrial Complex™. Of course, the real issue isn't antibiotic misuse-it's the systemic erosion of immune resilience through processed food, fluoride, and the complete abandonment of ancestral healing modalities. Did you know the Mayans used fermented honey to treat respiratory infections? No? Of course not. You're too busy scrolling through CDC bulletins.
Jonathan Morris
December 19, 2025 AT 08:19Let’s be precise: the claim that '99% of diarrhea and vomiting cases in children are viral' is statistically misleading. The CDC’s 2022 surveillance data shows 87.3% (CI 85.1–89.4%) for rotavirus and norovirus, with adenovirus and astrovirus accounting for most of the remainder. The 99% figure is a rhetorical flourish, not an epidemiological truth. Also, 'antibiotics are like hammers for leaky faucets'-poor analogy. Hammers don’t fix plumbing; pipe wrenches do. Analogies should be technically accurate or omitted.
Raven C
December 19, 2025 AT 19:18Oh, how utterly... *touching*. The gentle, paternalistic tone of this piece-'trust your body, be patient, wait 48 hours'-is so soothing, so reassuring, so... *bourgeois*. Meanwhile, single mothers working two jobs, with no paid sick leave, are being told to 'wait' while their child burns with fever. This isn’t medicine. It’s moralizing wrapped in clinical language. And don’t get me started on 'flavoring antibiotics'-as if the problem is taste, not systemic neglect.
BETH VON KAUFFMANN
December 20, 2025 AT 09:36Let’s not conflate correlation with causation. The 30% unnecessary antibiotic rate is a meta-analysis artifact. Real-world prescribing is far more nuanced. CRP-guided protocols reduce use, yes-but they also increase visit frequency and parental anxiety. And the 'watchful waiting' paradigm ignores socioeconomic variables: if you can’t afford to miss work, you’ll demand the script. This isn’t a clinical issue-it’s a structural one.
Jessica Salgado
December 20, 2025 AT 15:14I had no idea 80-90% of rashes aren’t allergies. My daughter broke out in red dots after amoxicillin and we were terrified. We avoided all penicillins for years. Then we did the skin test last year-turns out she’s fine. I cried. I literally cried. Thank you for saying this. So many kids are mislabeled. So many.
Sam Clark
December 22, 2025 AT 09:05Thank you for the thoughtful and evidence-based guidance. The emphasis on watchful waiting and accurate diagnostics is precisely what pediatric care needs. I have shared this with my colleagues in the family practice clinic. It is a valuable resource for parents who are seeking clarity amid overwhelming misinformation.
Donna Packard
December 23, 2025 AT 20:49This made me feel so much better. I used to panic every time my son got a cold. Now I just give him soup, hugs, and time. And I say no to antibiotics unless the doctor really means it. It’s not easy, but it’s right.
Patrick A. Ck. Trip
December 23, 2025 AT 23:25thank you for this post. i have a 4 year old and i was so scared of giving antibiotics but also scared of not giving them. this helped me understand the balance. i think doctors need to talk more like this. also, i didn't know about the flavoring thing-my kid hates medicine. i'm calling the pharmacy tomorrow.
Chris Van Horn
December 24, 2025 AT 20:01THIS IS THE MOST PATHETIC, NAIVE, AND DANGEROUS PIECE OF MISINFORMATION I'VE EVER READ. YOU WANT PARENTS TO 'WAIT'? WHAT IF THEIR CHILD DEVELOPS MENINGITIS BECAUSE YOU WERE TOO POLITE TO PRESCRIBE? YOU'RE NOT A DOCTOR. YOU'RE A BLOGGER WITH A BLOG. THE CDC ISN'T GOD. I'VE SEEN KIDS DIE BECAUSE OF YOUR KIND OF 'WATCHFUL WAITING'. YOU'RE KILLING CHILDREN WITH YOUR LIBERAL, HAND-HOLDING, 'TRUST NATURE' NONSENSE.
amanda s
December 25, 2025 AT 18:38AMERICA IS BEING DESTROYED BY OVER-EDUCATED PARENTS WHO THINK THEY KNOW MORE THAN DOCTORS. YOU WANT TO WAIT 48 HOURS? THEN WHY DO YOU HAVE HEALTH INSURANCE? JUST LET THEM SUFFER. THIS ISN’T A CHOICE-IT’S A CIVIL WAR ON MEDICINE. I’M TAKING MY KID TO A REAL DOCTOR WHO WILL PRESCRIBE WHAT’S NEEDED. NO MORE 'WATCHFUL WAITING'. NO MORE 'TRUST THE BODY'. MY CHILD ISN’T A LAB RAT FOR YOUR PHILOSOPHY.
Erik J
December 27, 2025 AT 18:21Interesting. I wonder how much of the resistance data is skewed by agricultural use. Livestock antibiotics are 70% of total usage. Maybe the real issue isn’t parents, but industrial farming. Just a thought.