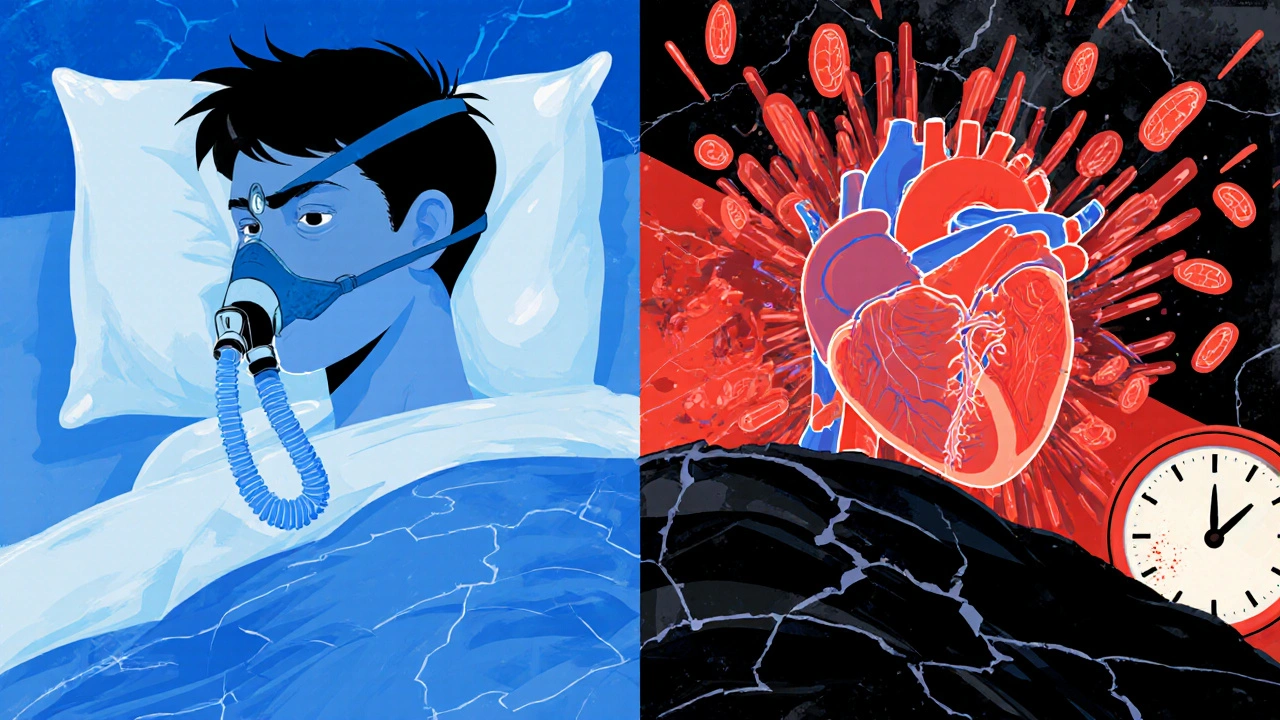
Every night, while you’re asleep, your body should be resting. But if you have sleep apnea, your breathing keeps stopping - sometimes dozens of times an hour. These pauses aren’t just annoying; they’re quietly damaging your heart. In fact, sleep apnea is one of the most overlooked causes of high blood pressure and heart disease, especially in people who think they’re otherwise healthy.
What Sleep Apnea Does to Your Body While You Sleep
Sleep apnea isn’t one condition - it’s mostly two. Obstructive sleep apnea (OSA) happens when your throat muscles relax too much and block your airway. Central sleep apnea is rarer and occurs when your brain fails to send the right signals to breathe. OSA makes up 80-90% of cases. And it’s not rare. Around 1 billion people worldwide have it, including 40 million in the U.S. alone.
What makes it dangerous isn’t just the snoring or the daytime tiredness. It’s what happens inside your body during those breath-holding episodes. Every time you stop breathing, your oxygen levels drop. Your body panics. Stress hormones like adrenaline spike - sometimes two to four times higher than normal. Your heart has to work harder. Blood pressure surges. And this doesn’t just happen once a night. It can happen 30, 50, even 100 times per hour.
The Link Between Sleep Apnea and High Blood Pressure
High blood pressure is the most common heart problem linked to sleep apnea. In fact, up to 80% of people with resistant hypertension - meaning their blood pressure stays high even after taking three different medications - also have undiagnosed sleep apnea.
But it’s not just about daytime numbers. Your blood pressure normally drops at night by 10-20%. That’s called “dipping.” It’s your body’s way of giving your heart a break. But in 70-80% of people with moderate to severe sleep apnea, this dip doesn’t happen. Their blood pressure stays high all night - or even rises. This pattern, called non-dipping or reverse-dipping, is a major red flag. It means your heart never gets true rest. And over time, that raises your risk of stroke, heart attack, and heart failure.
Studies show people with untreated sleep apnea are two to three times more likely to develop high blood pressure within just four to five years. And it’s not just older adults. A 2024 study of nearly 10,000 adults found that people aged 20-40 with sleep apnea symptoms were 45% more likely to have high blood pressure than their peers without it. That’s a big deal. It means sleep apnea isn’t just an aging problem - it’s accelerating heart disease in younger people.
How Sleep Apnea Fuels Heart Disease
High blood pressure is just the start. Sleep apnea also directly damages your arteries and heart muscle.
Repeated drops in oxygen trigger inflammation. Levels of C-reactive protein, a marker of body-wide inflammation, go up by 35-50% in people with OSA. Your blood vessels become stiff. The lining of your arteries - the endothelium - stops working properly. Flow-mediated dilation, a measure of how well your arteries relax, drops by 25-40%. That’s like having your arteries permanently clenched.
These changes raise your risk of coronary artery disease by 30%. If you have moderate to severe sleep apnea (AHI ≥15), you’re 1.3 times more likely to have a heart attack and 1.6 times more likely to die from one. What’s even more startling? About 26.5% of heart attacks in people with sleep apnea happen between midnight and 6 a.m. - the exact time when breathing pauses are most frequent.
And it doesn’t stop there. Sleep apnea increases your risk of heart failure by 140%. That’s because your heart is constantly overworked. The pressure swings inside your chest during apnea episodes force your heart to pump against higher resistance - up to 50% more than normal. Over years, this leads to thickened heart walls, reduced pumping power, and eventually, heart failure.
Stroke Risk Skyrockets
Stroke is another major threat. People with sleep apnea are 2.5 times more likely to have a first stroke. If you’ve already had one, your chance of having another jumps to 3.2 times higher. And the worse your nighttime oxygen levels drop - especially if your blood oxygen stays below 90% for more than 12% of your sleep time - the higher your risk of dying from a stroke. One study found that group had 4.3 times higher stroke mortality.
Why? Because the same stress on your blood vessels that causes heart attacks also causes clots and ruptures in the brain. And because your body is in constant fight-or-flight mode at night, your blood becomes stickier and more prone to clotting.
Arrhythmias: When Your Heart Goes Off-Rhythm
Heart rhythm problems are common in sleep apnea patients. You’re two to four times more likely to develop atrial fibrillation (AFib), the most common type of irregular heartbeat. In fact, nearly half of people with paroxysmal AFib - where the irregular rhythm comes and goes - also have untreated sleep apnea. That’s compared to just 21% of people without AFib.
And here’s the kicker: if you have AFib and sleep apnea, treatments like catheter ablation are 30% less likely to work. Your heart keeps getting shocked by the stress of apnea episodes, making it harder to restore normal rhythm. Even cardiac devices like pacemakers and resynchronization therapy respond worse if sleep apnea is left untreated.
Why Treatment Often Falls Short
Continuous Positive Airway Pressure (CPAP) is the gold standard treatment. It uses a mask to keep your airway open while you sleep. But here’s the problem: only 46% of people who use CPAP stick with it long-term. Most stop because it feels uncomfortable, noisy, or inconvenient.
And even when people use it regularly, the benefits aren’t always dramatic. CPAP typically lowers blood pressure by only 2-3 mmHg on average. That’s not much - but it’s enough to reduce stroke recurrence by 37% and improve heart failure outcomes, especially in central sleep apnea.
The bigger issue? Many doctors don’t screen for sleep apnea. If you have high blood pressure, heart failure, AFib, or have had a stroke - especially if treatment isn’t working - you should be tested. Yet, 80% of moderate to severe cases go undiagnosed.
What You Can Do Now
If you snore loudly, wake up gasping, feel exhausted during the day, or have high blood pressure that won’t budge - get tested. You don’t need a full overnight sleep lab study right away. Home sleep tests are 85-90% accurate for moderate to severe cases. They’re cheaper, easier, and can be done in your own bed.
Doctors are starting to use simple tools like the STOP-Bang questionnaire. It asks about snoring, tiredness, observed apneas, high blood pressure, BMI, age, neck size, and gender. It catches 84% of moderate to severe cases. If you score high, get a formal test.
And if you’re diagnosed? Don’t just accept CPAP as your only option. Weight loss helps - especially if you’re overweight. Losing just 10% of your body weight can cut apnea episodes by half. Sleeping on your side, avoiding alcohol before bed, and quitting smoking also make a difference.
The most important thing? Treat it. Sleep apnea isn’t just about poor sleep. It’s a silent driver of heart disease, stroke, and early death. Treating it doesn’t just help you sleep better - it saves your heart.
Who Should Be Screened?
Cardiologists now recommend screening for sleep apnea in anyone with:
- High blood pressure, especially if it’s resistant to medication
- Atrial fibrillation or other irregular heart rhythms
- Heart failure
- History of stroke or transient ischemic attack (TIA)
- Coronary artery disease
- Unexplained daytime fatigue despite enough sleep
- Obesity (BMI ≥30)
- Snoring with witnessed breathing pauses
And don’t wait until you’re 50. The data shows young adults with sleep apnea are at higher relative risk than older adults. If you’re under 40 and have these signs, don’t dismiss them as stress or laziness.
Can sleep apnea cause high blood pressure even if I’m young and healthy?
Yes. Even young, otherwise healthy people with sleep apnea are 45% more likely to develop high blood pressure than their peers without it. The stress on the body from repeated breathing pauses triggers hormonal and vascular changes that raise blood pressure - regardless of age or fitness level.
If I use CPAP, will my blood pressure go back to normal?
CPAP typically lowers blood pressure by only 2-3 mmHg on average, which may seem small. But for people with resistant hypertension, that drop can be enough to reduce stroke risk by 37% and improve heart function. It’s not a cure-all, but it’s a critical part of managing your overall cardiovascular risk.
Is sleep apnea linked to heart failure?
Yes. People with sleep apnea are 140% more likely to develop heart failure. The constant strain on the heart from low oxygen and pressure swings weakens the heart muscle over time. Also, 40-60% of people already diagnosed with heart failure also have undiagnosed sleep apnea - making it a two-way problem.
Can losing weight fix sleep apnea?
For many people, yes. Losing just 10% of your body weight can reduce sleep apnea episodes by half. Since obesity is linked to 70% of obstructive sleep apnea cases, weight loss is one of the most effective non-device treatments - especially when combined with CPAP or positional therapy.
Why do I need to get tested if I don’t feel that tired during the day?
Many people with sleep apnea don’t feel sleepy during the day. Instead, they might have brain fog, morning headaches, irritability, or just feel like they’re not recovering from sleep. But the real danger isn’t how you feel - it’s the silent damage to your heart and blood vessels. Even without daytime symptoms, untreated sleep apnea increases your risk of stroke, heart attack, and early death.


Corra Hathaway
November 21, 2025 AT 16:11Okay but like… why is everyone acting like this is news? I’ve been snoring like a chainsaw since college and my doc just shrugged. Now my BP’s through the roof. 🙄 Time to finally get that home test. No more ‘it’s just stress’ nonsense.
Swati Jain
November 22, 2025 AT 15:53From an Indian cardiology perspective: OSA is the silent epidemic in our urban population. 70% of hypertensive patients here have undiagnosed OSA. The STOP-Bang questionnaire? Works like a charm. But access to CPAP? Still a luxury. We need decentralized screening-community health workers, mobile units, not just tertiary hospitals. Also, yoga + pranayama reduces AHI by 30% in mild cases. Evidence-backed, folks.
Florian Moser
November 22, 2025 AT 17:31It’s not just about CPAP compliance-it’s about understanding the pathophysiology. Repeated hypoxia triggers sympathetic overactivation, endothelial dysfunction, and systemic inflammation-all measurable biomarkers. The 2–3 mmHg BP reduction with CPAP isn’t trivial; it’s clinically significant when applied population-wide. Studies show a 10% reduction in cardiovascular events for every 5 mmHg sustained drop. This isn’t anecdotal. It’s physiology.
jim cerqua
November 23, 2025 AT 23:06LET ME TELL YOU SOMETHING. MY DAD DIED AT 52. HE SNORED. HE HAD HIGH BP. THEY SAID IT WAS ‘OLD AGE.’ TURNED OUT HE HAD SEVERE SLEEP APNEA FOR 12 YEARS AND NO ONE CHECKED. THEY GAVE HIM MORE MEDS. NEVER ASKED ABOUT SLEEP. I’M NOT JUST MAD-I’M FURIOUS. THIS ISN’T A MEDICAL ISSUE-IT’S A SYSTEMIC FAILURE. THEY’RE KILLING US WITH NEGLECT. AND NOW I’M TESTING MYSELF. IF YOU’RE READING THIS AND YOU SNORE? DO IT. NOW. DON’T WAIT FOR THE HEART ATTACK.
Donald Frantz
November 25, 2025 AT 03:35Where’s the data on CPAP improving long-term mortality in young adults? Most studies focus on elderly populations with comorbidities. The 45% increased BP risk in 20–40-year-olds sounds alarming, but is it causal or correlational? What about confounders like screen time, sedentary behavior, or sugar intake? I’m not dismissing sleep apnea-but we need better longitudinal data before we turn every snorer into a cardiac patient.
Sammy Williams
November 26, 2025 AT 14:16Just got my home test results-moderate OSA. Started CPAP last week. First night felt like wearing a space helmet. Second night? Slept like a baby. Woke up without my 3 p.m. crash. My wife says I stopped sounding like a foghorn. Worth every awkward minute. Also lost 8 lbs just because I’m not exhausted all day. Small wins, y’all.
Julia Strothers
November 28, 2025 AT 04:09Who’s funding this? Big Pharma? CPAP machines cost $3K. Sleep labs? $5K. Meanwhile, the FDA approves new BP pills every year. Coincidence? Or is this a multi-billion-dollar industry built on making people dependent on machines while ignoring root causes like toxins, EMFs, and government-approved food additives? Wake up. Sleep apnea isn’t a medical condition-it’s a symptom of a poisoned system.
Erika Sta. Maria
November 29, 2025 AT 07:39But… what if sleep apnea is just nature’s way of forcing us to confront our existential dread? I mean, think about it-our breath stops because we’re too attached to control. The body rebels. The heart races because the soul is screaming. Maybe we need meditation, not masks. Maybe the real cure is surrendering to the void. Also, I think my neighbor’s WiFi is causing my apnea. I checked. My neck is 17 inches. That’s not obesity. That’s destiny.