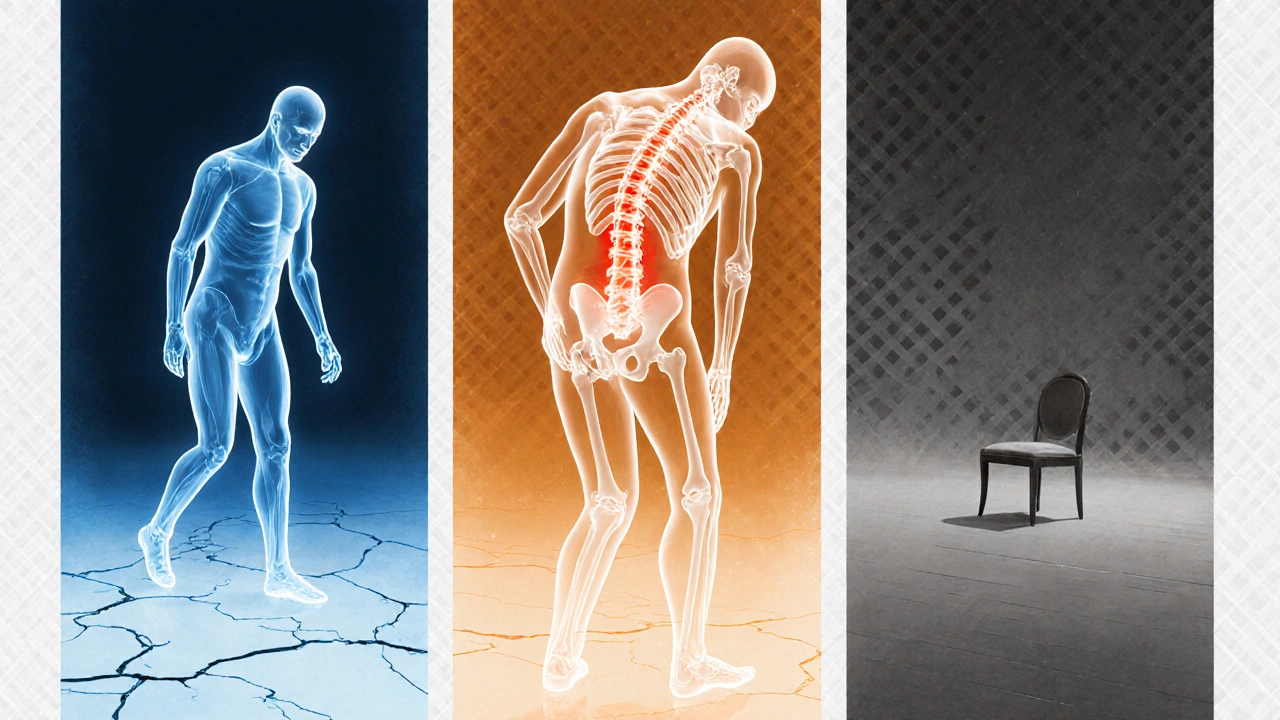
Osteoporosis & Mental Health Symptom Checker
Psychological Symptoms
- Persistent Sadness Mental
- Fear of Falling Mental
- Social Withdrawal Mental
- Sleep Disturbances Mental
- Anxiety Spikes During Doctor Visits Mental
Physical Symptoms
- Reduced Bone Density Physical
- Vertebral Compression Fractures Physical
- Limited Range of Motion Physical
- Chronic Back Pain Physical
- Increased Calcium Excretion Physical
Research shows that psychological symptoms often stem from physical changes associated with osteoporosis:
- Fear of Fracture Risk: Constant vigilance about falls can drain emotional energy.
- Pain and Mobility Limits: Chronic back pain contributes to depressive states.
- Social Identity Shift: Reduced participation in social activities can lower self-worth.
Select a symptom above and click "Check Symptom Connection" to see how it relates to mental health and physical symptoms.
Living with osteoporosis isn’t just about fragile bones. The daily reality of monitoring bone density, fearing a fall, and adjusting activities can weigh heavily on the mind. When the condition stretches out over years, it often sparks a cascade of emotional reactions-worry, sadness, even anger. This article breaks down the most common psychological effects, shows how they connect to the physical side of the disease, and offers practical ways to keep both body and mind in better shape.
Why the Mind Feels the Impact
At its core, osteoporosis is a chronic condition that silently progresses until a fracture reminds you it’s there. That uncertainty fuels a stress response. The body releases cortisol, the hormone that prepares you to fight or flee. Over time, elevated cortisol can dampen mood, blur concentration, and make it harder to enjoy daily activities.
Typical Psychological Symptoms
Research shows that up to 30% of people with osteoporosis experience clinically significant mood changes. The most frequently reported signs include:
- Persistent sadness or feelings of hopelessness
- Excessive worry about falling or breaking a bone
- Loss of interest in hobbies that once brought joy
- Sleep disturbances-either insomnia or restless nights
- Social withdrawal because of embarrassment or fear
These symptoms often overlap with depression and anxiety, making it crucial to differentiate whether the mood shift stems from the disease itself or a separate mental‑health condition.
How Physical Changes Trigger Emotional Shifts
There are three main pathways that link bone loss to mental health:
- Fear of Fracture Risk: Knowing that a minor slip could lead to a major break creates constant vigilance. That hyper‑awareness drains emotional reserves.
- Pain and Mobility Limits: Even before a fracture, many people report chronic back pain from vertebral compression. Ongoing pain is a well‑established driver of depressive states.
- Social Identity Shift: When you can’t participate in group sports, dance classes, or even simple outings, the sense of self‑worth can erode.
Understanding these connections helps you spot the early warning signs before they snowball.
Spotting When Professional Help Is Needed
Not every low mood requires a therapist, but certain red flags demand attention:
- Feelings of worthlessness that last more than two weeks
- Thoughts of self‑harm or suicide
- Inability to perform everyday tasks because of fear
- Persistent insomnia despite good sleep hygiene
If you tick any of these boxes, reaching out to a mental‑health professional can prevent a deeper crisis. Many clinics now offer integrated services where a support group therapist works alongside an endocrinologist or rheumatologist.
Practical Strategies to Protect Your Mental Well‑Being
Below are real‑world tactics that have helped people keep their spirits up while managing osteoporosis:
- Educate Yourself: Knowledge reduces fear. Learn what bone‑density scores mean, which foods boost calcium, and which exercises are safe. A clear picture replaces vague dread.
- Stay Active Within Limits: Weight‑bearing activities like brisk walking or low‑impact aerobics improve both bone health and mood‑boosting endorphins. Use a support cane or handrail if needed.
- Practice Mindfulness: Simple breathing exercises, guided meditations, or yoga (modified for balance) calm the cortisol surge and sharpen focus.
- Build a Community: Join an online forum or a local support group. Sharing stories normalizes the experience and offers new coping ideas.
- Keep a Mood Journal: Track triggers, sleep patterns, and pain levels. Over time you’ll see patterns that suggest which adjustments work best.
- Seek Professional Guidance Early: A psychologist familiar with chronic illnesses can teach cognitive‑behavioral techniques tailored to fracture‑related anxiety.

Comparison of Common Psychological Effects vs. Physical Symptoms
| Psychological | Physical |
|---|---|
| Persistent sadness | Reduced bone density (T‑score ≤ -2.5) |
| Fear of falling | Vertebral compression fractures |
| Social withdrawal | Limited range of motion in hips/knees |
| Sleep disturbances | Chronic back pain |
| Anxiety spikes during doctor visits | Increased calcium excretion |
Resources You Can Turn to Right Now
Below is a quick checklist of things you might keep on hand:
- National Osteoporosis Foundation website - reliable facts and exercise videos
- MindSpot (Australia) - free online CBT modules for anxiety and depression
- Local library - “Living Well with Osteoporosis” book series
- Pharmacy‑based bone‑health consultations - often free with a prescription
- Community centre - senior‑focused balance classes (many are subsidised)
Frequently Asked Questions
Can osteoporosis cause depression even if I haven’t broken a bone?
Yes. The constant awareness of fracture risk, changes in mobility, and the hormonal stress response can all lower mood, independent of an actual fracture.
Is anxiety more common than depression in osteoporosis patients?
Studies show anxiety slightly edges out depression, especially in the first two years after diagnosis, because fear of falling dominates early coping.
Do calcium supplements affect my mood?
Calcium itself isn’t a mood regulator, but low calcium can exacerbate muscle cramps and sleep problems, which indirectly worsen mood.
Should I see a psychologist if I only feel occasional worry?
Occasional worry is normal. However, if the worry interferes with daily plans, joins forces with sleeplessness, or lasts more than a month, a brief consultation can help you develop coping tools before it escalates.
What role do support groups play in mental health?
Sharing experiences reduces isolation, provides practical tips, and often introduces members to mental‑health professionals who specialize in chronic illness.


Taryn Thompson
October 11, 2025 AT 12:07Thanks for pulling together the bone‑health and mood link in one place.
Lisa Lower
October 16, 2025 AT 18:47I love how you laid out the facts, it really helps people see the whole picture. The way you tied fear of falling to cortisol spikes is spot on. It’s also great that you listed practical steps right after the science. Readers can actually use this info right away, which isn’t always the case with health posts. Keep the good work coming, and maybe add a quick printable checklist for daily bone‑health habits.
Dana Sellers
October 22, 2025 AT 01:27Honestly, if you’re not taking this seriously you’re just being lazy. People need to understand that ignoring bone loss will wreck their mood for good.
Damon Farnham
October 27, 2025 AT 07:07Well, this is a comprehensive overview, however, I must point out that the emphasis on “fear of falling” seems a bit overstated; many patients, especially in our region, exhibit resilience, yet the article glosses over cultural coping mechanisms, which is a glaring omission; nonetheless, the data is solid, the writing is crisp, and the tables are useful.
Gary Tynes
November 1, 2025 AT 13:47great info but watch out for typos… also, try to split the long paragraphs into bite‑size chunks its easier to read.
Marsha Saminathan
November 6, 2025 AT 20:27Reading through this article feels like taking a guided tour through a museum of bone‑related anxiety and optimism, where each exhibit is meticulously labeled and the curator has clearly spent countless hours polishing the plaques. First, the opening paragraph instantly grabs attention, painting a vivid picture of how a silent disease can shout loudly in the mind. Then, the symptom checker graphic is a brilliant way to merge interactivity with education, allowing users to see the direct line from a cracked vertebra to a sleepless night. The author wisely explains cortisol’s role, not just as a stress hormone but as a molecular bridge between physical fragility and emotional turbulence, which is something most laypeople never hear about. I love how the piece doesn’t just stop at theory; it offers concrete suggestions like weight‑bearing exercise, mindfulness practices, and community support groups, each backed by a brief explanation of how they can actually fortify both bone and spirit. The table comparing psychological and physical symptoms is crystal‑clear, using simple language without sacrificing nuance, which is a rare achievement in medical writing. The FAQ section anticipates the reader’s doubts, especially the question about calcium's effect on mood, providing a balanced answer that demystifies common myths. Throughout, the tone stays empathetic yet empowering, never slipping into fatalism, which is essential for maintaining hope in chronic illness. Moreover, the resource list at the end gives a handy roadmap for further reading, from the National Osteoporosis Foundation to free CBT modules, showing a genuine commitment to holistic care. In short, this article succeeds on every front: education, engagement, and empowerment, making it a model for how health content should be crafted. Kudos to the author for such a thorough and compassionate piece!
Justin Park
November 12, 2025 AT 03:07Great blend of science & practical advice 😊. The way you tie cortisol to mood really shows the mind‑body connection. Keep the emojis coming for a light touch!
Herman Rochelle
November 17, 2025 AT 09:47Very helpful overview. The suggestions are clear and actionable.
Stanley Platt
November 22, 2025 AT 16:27Impressive depth of research; however, one might consider adding a brief summary for readers pressed for time-perhaps a bullet‑point recap? 🤔; this would enhance accessibility while preserving the article’s scholarly rigor.
Alice Settineri
November 27, 2025 AT 23:07Whoa, this article is like a rollercoaster of facts and feels! I’m vibing with the part about dancing around fear-let’s literally dance, people! 🎉
nathaniel stewart
December 3, 2025 AT 05:47Ths articl is vry informativ, thnk you for the dtailed explantion. Pls keep up the gd work!
Pathan Jahidkhan
December 8, 2025 AT 12:27Ah, the tragedy of brittle bones-how the very marrow of our flesh echoes in the chambers of our mind. One feels the weight of each vertebra like a whispered accusation from fate itself. Yet, amidst that gloom, there lies a spark, a call to arms for the spirit to rise above the creaking scaffolding of the body.
Dustin Hardage
December 13, 2025 AT 19:07Indeed, the poetic framing captures the existential burden of osteoporosis while remaining grounded in clinical evidence. Your delineation of cortisol pathways aligns well with current endocrinological literature, and the recommendation for integrative therapy is both pragmatic and evidence‑based.
Dawson Turcott
December 19, 2025 AT 01:47Wow, another article telling us to “exercise more.” 🙄 As if the world isn’t already full of people who can’t find time to stretch a toe. Maybe add a section on how to do it while binge‑watching Netflix?
Alex Jhonson
December 24, 2025 AT 08:27Appreciate the balanced perspective. It’s useful to see both medical and community resources side by side.
Katheryn Cochrane
December 29, 2025 AT 15:07The article seems overly optimistic; real patients often feel isolated despite these tips.
Michael Coakley
January 3, 2026 AT 21:47Sure, “optimism” works if you’re not dealing with constant pain. Reality check: most folks just want relief, not pep talks.
ADETUNJI ADEPOJU
January 9, 2026 AT 04:27While the discourse adopts a layman’s vernacular, the underlying pathophysiology warrants a more rigorous, jargon‑laden exposition to satisfy the specialist cohort.
Janae Johnson
January 14, 2026 AT 11:07I’m not convinced the link between calcium excretion and mood is that strong; seems like a stretch to me.