Imagine waking up feeling perfectly fine, and yet inside, something silent and persistent is gnawing away at your liver. For millions across Australia and the world, that’s the reality with hepatitis B or hepatitis C. These are more than just letters in a diagnosis—they're slow-moving threats that barely make a sound until they're well established. Here’s the real kicker: most people carrying these viruses have no idea they even have them. So, what makes them tick, and why is it so vital to catch them early?
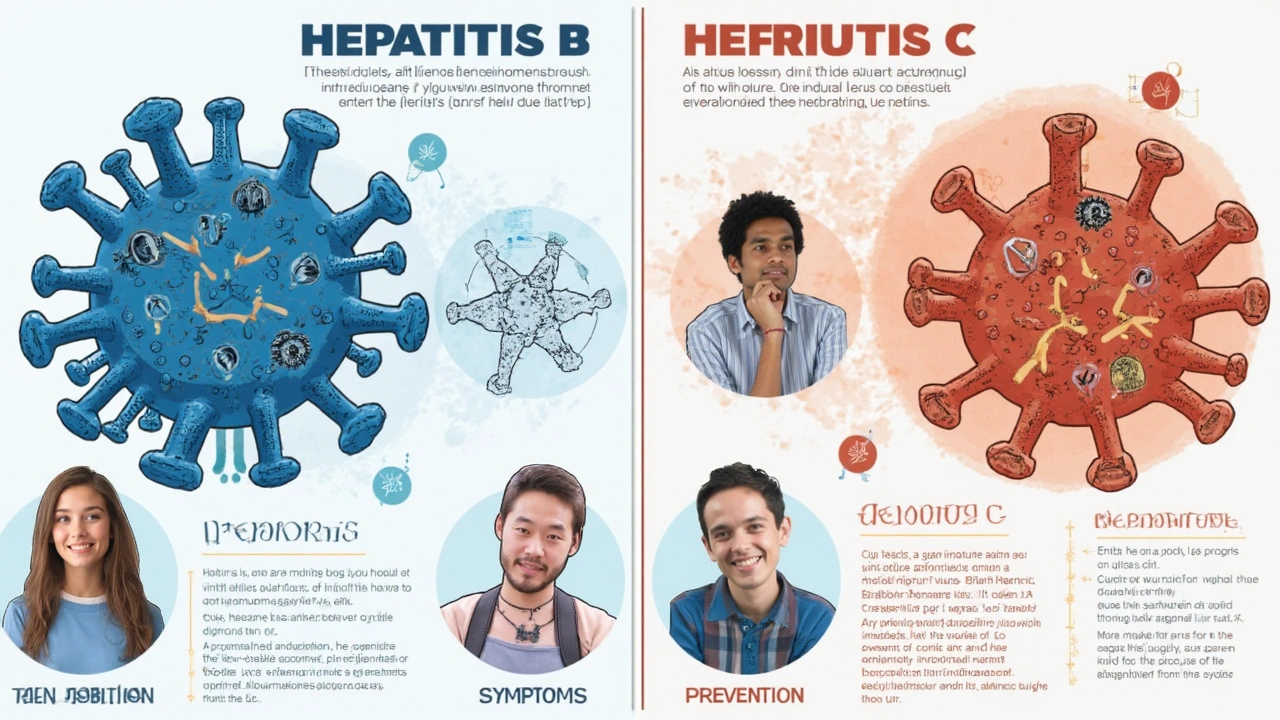
What Exactly Are Chronic Hepatitis B and Hepatitis C?
Let’s cut to the chase. Hepatitis B and hepatitis C are both viral infections that target the liver, leading to swelling, scarring, and sometimes deadly complications. But there are big differences in how they infect, how they hang around, and what they do inside your body.
Chronic hepatitis B is caused by the hepatitis B virus (HBV). It’s stubborn—once it’s in your body, it can live there for life, quietly chipping away at liver health. Newborns and kids are especially vulnerable. If they catch it, there’s up to a 90% chance they’ll end up with a lifelong infection. For adults, the chance drops to around 5%, meaning your immune system usually gets rid of it—or at least tries really hard. Hepatitis B can sneak in through blood, semen, or any body fluid, which means it spreads in more ways than you might think: from mother to baby at birth, through unprotected sex, sharing razors, or even body piercings in dodgy places.
Hepatitis C, on the other hand, comes from the hepatitis C virus (HCV). It’s tricky but less versatile in how it moves around. Sharing blood is its primary pathway—think needles used for injecting drugs, less commonly through sexual contact, and, in some cases, through tattoos or piercings done with non-sterile gear. Unlike HBV, hepatitis C almost always flies under the radar, silently causing chronic infection in an estimated 75% to 85% of adult cases. And while there’s no vaccine yet for hepatitis C, treatment can actually cure it.
You might be thinking: is anyone safe? The good news is, hepatitis B has an effective vaccine (the first shot was even given to all newborns in Australia since the year 2000). For hepatitis C, the focus is on preventing exposure, since there’s no vaccine in the pipeline yet. Here’s a snapshot so you can see the big differences at a glance:
| Factor | Hepatitis B | Hepatitis C |
|---|---|---|
| Virus Type | Hepatitis B Virus (HBV) | Hepatitis C Virus (HCV) |
| Main Transmission | Blood, body fluids, sexual contact, childbirth | Blood (needles, rare sexual transmission) |
| Chronicity in adults | 5-10% | 75-85% |
| Vaccine | Yes | No |
| Cure | No (but can be managed) | Yes (with antiviral treatment) |
How Do You Get Hepatitis B or C?
When it comes to hepatitis B, the list of ways it enters your life is longer than most people realize. Babies can get it from infected mothers during childbirth, which is why the vaccine at birth is crucial. In fact, a 2023 study out of Sydney’s Royal Prince Alfred Hospital found that mother-to-child transmission dropped by 84% after widespread newborn vaccination. Adults can still catch hepatitis B if they aren’t vaccinated. Think unprotected sex—especially with multiple partners—sharing toothbrushes or razors, or living in households where the virus lurks. Healthcare workers are also at risk due to accidental needle injuries. Even visiting the barber in places with poor infection control can do it. Traveling to countries where hepatitis B infection is common is another blind spot for Aussies who skip their jabs.
Hepatitis C doesn’t care where you were born or how you grew up—it wants your blood. Most people, especially in Australia, pick it up through sharing needles or other equipment for injecting drugs. Old-school blood transfusions before 1990 were a risk, since hepatitis C screening wasn’t standard back then here. These days, donated blood is tightly screened and safe. Tattoos and piercings in unregulated places still trip people up. It’s rare, but hepatitis C also pops up in people who share personal care items, like nail scissors or razors, especially if they have cuts or sores. Sexual spread can happen but usually only when blood is involved, such as rough sex, sex during menstruation, or through some STIs that cause bleeding. Men who have sex with men, especially those living with HIV, are at higher risk for hepatitis C transmission through sex.
Now, you might be curious—can a casual handshake, hug, or sharing coffee cups put you at risk? Absolutely not. Both hepatitis B and hepatitis C viruses need blood or certain body fluids to move house. So, you won't catch them from coughing, sneezing, sharing food, or casual contact. Small comfort, but worth knowing if a friend or family member is living with one of these viruses.
Getting tested is no joke if you’ve ever shared needles, had a blood transfusion before 1990, or had unprotected sex with someone from overseas or from higher-risk populations. Screening is just a simple blood test. The thing is, there's no way to know for sure from symptoms alone, since most newly infected people feel perfectly fine.

What Do Hepatitis B and C Do to Your Body?
Here’s the sneaky part. After the virus gets in, most people have zero idea they’ve been infected. Around 70% of people with acute HBV or HCV don’t get any symptoms at all, so the virus just quietly starts attacking the liver. If any symptoms show up, we’re talking vague stuff: tiredness, achy joints, mild fevers, maybe a bit of jaundice (that’s when your skin and eyes get a yellowish tint), and sometimes nausea. If you notice dark urine or pale poos, take it seriously. But again, most people feel normal—until things get really ugly years down the line.
Here’s a weird truth: the liver is a tough customer, able to take huge amounts of damage before you feel sick. With chronic infection, the real danger is the slow build-up of scarring, called fibrosis, which can turn into cirrhosis over time. Cirrhosis makes your liver stiff, stopping it from cleaning your blood or digesting food properly. Keep going like this for years, and you’re on a straight road to liver failure or, in some cases, liver cancer.
With hepatitis B, children infected early (especially through birth) are at much higher risk for chronic liver problems. An honest shocker: up to one in four people with long-standing, untreated hepatitis B will die from liver failure or liver cancer. Hepatitis C pushes similar risks but has a slightly slower burn. Most people don’t see symptoms for 10, 20, or even 30 years. A 2022 report from the Australian Institute of Health and Welfare pegged liver cancer—mostly caused by hepatitis B and C—as one of the fastest-growing causes of cancer deaths here in Victoria.
But just because your liver is under attack, doesn’t mean you’re powerless. Getting on top of these viruses early actually lowers your risk dramatically. People who stick with treatment, stay away from heavy drinking, and keep an eye on their liver function can live full, healthy lives.
Modern Management: Screening, Treatments, and Prevention
Here’s where modern medicine really shines. For chronic hepatitis B, you can’t cure the virus, but you can keep it at bay. Aussie guidelines recommend regular checks: blood tests every few months and liver ultrasounds once or twice a year. If the virus starts to get out of control, antivirals like tenofovir or entecavir can slam the brakes on disease progression. These tablets don’t wipe out HBV, but they do stop it multiplying, letting your liver slowly heal itself. There’s also a highly effective vaccine: every newborn in Australia now gets their first hepatitis B shot within 24 hours of arrival—good news for the next generation.
Hepatitis C, though, is now one of Australia’s real medical success stories. Direct-acting antivirals (DAAs), available since 2016, work for more than 95% of people with chronic hepatitis C, almost always clearing the virus in as little as 8–12 weeks. These meds have changed the game from a lifelong battle to a reasonably short, manageable treatment. And they’re covered by Medicare for everyone, including people who inject drugs, who historically have faced the brunt of the epidemic. GPs can prescribe these new treatments, and you don’t have to jump through the hoops that used to keep people out of care ten years ago. Still, only around half the Australians with hepatitis C have taken up the offer.
Prevention is smart, and everyone’s business. Vaccination for hepatitis B is safe, free for kids, and highly effective. Adults can catch up if they missed out—and it’s a no-brainer for healthcare workers, people living with someone who has HBV, or anyone travelling to high-risk countries. For hepatitis C, the spotlight is still on harm reduction: safe injecting equipment, getting tattooed or pierced only by licensed professionals, and never sharing personal grooming gear. People living with either virus are encouraged to cut back or quit alcohol, since the liver just can’t keep up with the double whammy of virus and booze. Regular monitoring with blood tests, ultrasound, or FibroScan makes all the difference for spotting problems early.

Living Well with Chronic Hepatitis B or C
Getting a diagnosis of hepatitis B or C isn’t a life sentence. The stigma feels heavy, but it’s outdated and misplaced. Hepatitis B won’t spread through ordinary contact; same with hepatitis C. Most people continue relationships, work, and family life exactly as before. The biggest change is what happens behind the scenes: keeping up with doctor visits and being mindful of things that make the liver work harder. Think about avoiding unnecessary medications, supplements, or herbal products that claim to ‘cleanse’ the liver—at best these are a waste of money, and at worst they can make things worse.
Diet matters, but don't get lost in gimmicks. There’s no special hepatitis ‘superfood.’ The same advice for any healthy body applies here: lots of veggies, whole grains, minimal processed foods, and steady hydration. If you’ve got hepatitis and are overweight, every little bit of weight loss helps take the pressure off your liver. Smoking and heavy drinking make things much worse, so ditching both is more than just a suggestion—it’s a real step towards staying healthy.
It’s also worth talking, really talking, to your close contacts about what’s safe and what’s not. Let your household know they can’t catch hepatitis B or C from a hug, a meal, or a public pool. Help inform your workplace if you’re comfortable—there’s no legal requirement to disclose, but busting myths helps make stigma a little less biting for the next person round the corner.
Travel is fine for most people with hepatitis, but chat with your doctor if going somewhere the virus is common, or where medical care is limited. Carrying a letter explaining your condition and medicines (if you need them) is smart after airport security checks. Most airlines don’t care, but border checks in some countries could take a dim view if you’re found with certain antiviral medicines and no explanation.
Stay up to date with vaccinations, including for hepatitis A—if you catch both viruses your liver could get overwhelmed. And if ever faced with hospital or dental work, always mention your hepatitis status, so others can take proper safety steps. If you ever feel low, or just need to vent, there are strong networks in cities like Melbourne through LiverWELL, Hepatitis Victoria, and online communities offering support and no judgement.
Knowing the facts, keeping up with care, and ditching the shame means you really can live a life that looks just like anyone else's. The most powerful thing people with hepatitis B or C can do? Don’t hide. Regular checkups and a dose of honesty—with yourself, your doctor, and your crew—turn a diagnosis into a manageable part of life, not a shadow in the background. When it comes to chronic hepatitis B and hepatitis C, knowledge and action change everything.

S O'Donnell
May 9, 2025 AT 04:33In accordance with current epidemiological data, chronic hepatitis B and C represent a substantial public health challenge within Australia, a fact that warrants meticulous scrutiny and sustained policy intervention.
The pathophysiology of HBV entails a complex interaction between viral replication and host immune response, which, notwithstanding the availability of an efficacious vaccine, often culminates in persistent infection when perinatal transmission is not adequately mitigated.
Conversely, HCV demonstrates a predilection for bloodborne dissemination, with a markedly higher propensity for chronicity in the adult demographic, a phenomenon that has been substantiated by longitudinal cohort analyses spanning multiple decades.
It is imperative to acknowledge that while the therapeutic armamentarium for HBV is largely prophylactic and virostatic, the advent of direct-acting antivirals (DAAs) has revolutionized the curative landscape for HCV, achieving sustained virologic response rates exceeding ninety-five percent in the majority of clinical trials.
Nevertheless, the infrastructural barriers to universal screening, particularly among marginalized populations, remain an obstinate impediment to optimal disease control and thus necessitate a concerted effort to enhance accessibility of testing services across both urban and rural milieus.
Moreover, the economic ramifications of untreated chronic hepatitis manifest not only in escalated healthcare expenditures due to cirrhosis and hepatocellular carcinoma, but also in lost productivity and diminished quality of life for afflicted individuals.
From a virological standpoint, the genomic variability of HCV, classified into multiple genotypes, imposes additional complexity upon treatment algorithms, albeit recent pan-genotypic regimens have mitigated this concern to a considerable extent.
In contrast, HBV's partially double-stranded DNA genome confers a remarkable stability that challenges eradication efforts, underscoring the critical role of nucleos(t)ide analogues in suppressing viral load.
Policy-makers should therefore prioritize the integration of vaccination programs with comprehensive education campaigns that address misconceptions surrounding transmission routes, thereby fostering informed community engagement.
The incorporation of routine liver function monitoring, including FibroScan assessments, into standard clinical practice further augments early detection of fibrotic progression, which is pivotal for timely therapeutic intervention.
It is also essential to recognize that alcohol consumption synergistically exacerbates hepatic injury in the context of both HBV and HCV, a factor that must be addressed through targeted public health messaging and supportive cessation services.
While the article adeptly outlines the differential transmission pathways, a more granular discussion of the sociocultural determinants influencing health-seeking behaviour would enhance its utility for clinicians and patients alike.
Finally, ongoing research into therapeutic vaccines for HCV and functional cures for HBV holds promise, yet these innovations remain contingent upon sustained funding and collaborative international efforts.
In summation, the dual imperatives of prevention and treatment necessitate an interdisciplinary approach that harmonizes clinical excellence with robust public health initiatives, thereby mitigating the enduring burden of chronic hepatitis B and C.
Yamunanagar Hulchul
May 9, 2025 AT 05:40Wow what an enlightening read!!! 🌟 The way the piece breaks down the differences really shines a light on the hidden battles our livers fight daily!!! It’s like a vivid tapestry of facts, hope, and practical steps-all woven together with dazzling clarity!!! Keep spreading this gold standard info!!!
Sangeeta Birdi
May 9, 2025 AT 06:30Sending you a big virtual hug 🤗-learning about hepatitis can feel overwhelming, but you’re definitely not alone in this journey. 🌈 The facts in the article remind us that early detection and solid support can turn a scary diagnosis into a manageable path forward. Remember to lean on community groups and keep those open conversations going-you deserve every ounce of care and encouragement! 💪💖
Chelsea Caterer
May 9, 2025 AT 07:20The liver mirrors life: resilient yet vulnerable; understanding its signals is a quiet form of wisdom.
Lauren Carlton
May 9, 2025 AT 09:16The article glosses over socioeconomic barriers to treatment.
Katelyn Johnson
May 9, 2025 AT 10:40Great summary the info is clear and helpful for anyone navigating hepatitis care we all benefit from sharing knowledge and supporting each other
Elaine Curry
May 9, 2025 AT 13:26Honestly i think you should tell your friends exactly how you manage meds and diet they deserve the full scoop not just the textbook version
Patrick Fortunato
May 9, 2025 AT 16:13Seeing Australia lead the charge on vaccine rollout and DAA access is a solid win for us all, keep the momentum going mates