Many older adults take medications every day to manage pain, allergies, overactive bladder, or depression. But what if some of those everyday pills are quietly harming their memory and thinking? That’s the reality of anticholinergic burden-a hidden risk that’s quietly affecting millions of seniors.
What Exactly Is Anticholinergic Burden?
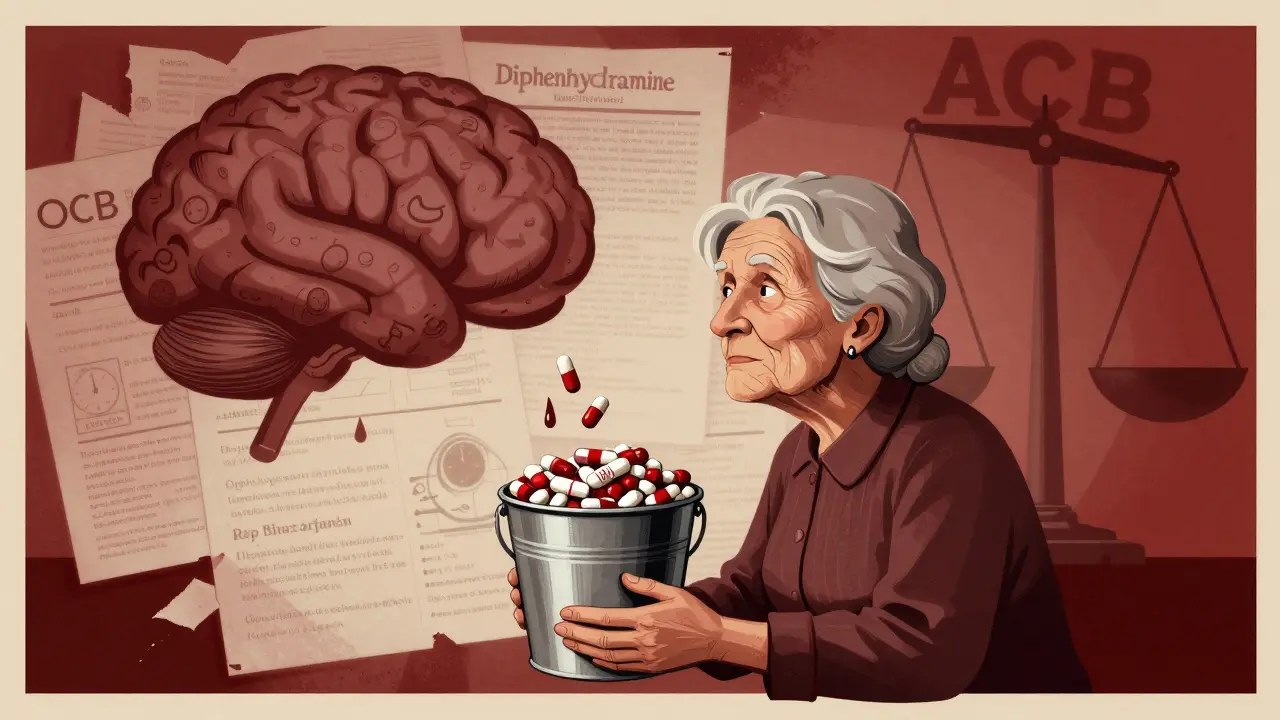
Anticholinergic burden is the total effect of all the medications a person takes that block acetylcholine, a brain chemical critical for memory, attention, and learning. It’s not about one drug-it’s about the cumulative impact of multiple drugs, even if each one seems harmless on its own. Think of it like filling a bucket with water. One cup of water won’t spill over. But keep adding cups-diphenhydramine from allergy pills, oxybutynin for bladder control, amitriptyline for sleep or pain-and eventually, the bucket overflows. In the brain, that overflow shows up as confusion, forgetfulness, and slower thinking. The most widely used tool to measure this is the Anticholinergic Cognitive Burden (ACB) scale. It rates each drug from Level 1 (mild) to Level 3 (strong). A person taking two Level 2 drugs and one Level 3 drug has an ACB score of 7. Research shows that scores of 3 or higher are linked to measurable cognitive decline.Which Medications Carry the Highest Risk?
Not all anticholinergic drugs are the same. Some are obvious-like Benadryl or older antidepressants. Others are less known, even to doctors.- First-generation antihistamines: Diphenhydramine (Benadryl), chlorpheniramine. Used for allergies, colds, or sleep. These cross the blood-brain barrier easily and are among the most common culprits.
- Overactive bladder drugs: Oxybutynin, tolterodine, solifenacin. Oxybutynin is a Level 3 drug-strong anticholinergic effect. Many seniors take it for years without knowing the brain risks.
- Tricyclic antidepressants: Amitriptyline, nortriptyline. Still prescribed for nerve pain or depression, even though safer SSRIs exist.
- Anti-Parkinson’s and antipsychotics: Benztropine, clozapine. Used less often, but still carry high ACB scores.
How Do These Drugs Actually Hurt the Brain?
Acetylcholine isn’t just a chemical-it’s the brain’s main signal for memory formation and focus. The M1 muscarinic receptors, where anticholinergics block this signal, are packed in the hippocampus and frontal cortex-areas responsible for remembering names, planning tasks, and staying focused. Brain scans tell a clear story. A 2016 study in JAMA Neurology found that older adults taking medium-to-high ACB drugs had 4% less glucose metabolism in the temporal lobe-the same region that shrinks in early Alzheimer’s. Even people without dementia showed this pattern. MRI studies from the Indiana Memory and Aging Study showed that long-term users of anticholinergics had brain shrinkage rates 0.24% faster per year than non-users. That might sound small, but over five years, it adds up to noticeable structural changes. And it’s not just structure-it’s function. The ASPREE study, which followed nearly 20,000 seniors over nearly five years, found that each 1-point increase in ACB score led to:- 0.15-point greater decline per year in executive function (planning, problem-solving)
- 0.08-point greater decline per year in verbal memory (remembering lists or stories)

Long-Term Use = Higher Dementia Risk
The biggest fear? That these drugs might not just cause temporary confusion-but actually increase the chance of developing dementia. A landmark 2015 study in JAMA Internal Medicine tracked over 3,400 older adults for more than a decade. Those who took strong anticholinergic drugs for three years or more had a 54% higher risk of dementia than those who used them for less than three months. Even after adjusting for other health conditions, the link held strong. This isn’t just correlation. The dose-response pattern is clear: more drugs, longer use, higher risk. And it’s not reversible overnight. The brain doesn’t bounce back in a week. The DICE trial showed that after 12 weeks of stopping anticholinergics, seniors saw small but meaningful improvements in cognitive test scores. But full recovery can take months-or may never be complete if damage has been long-standing.Real People, Real Consequences
Behind the statistics are real lives. One caregiver on AgingCare.com wrote: “My mom was constantly confused, forgetting meals, mixing up names. We thought it was early dementia. Then her pharmacist flagged oxybutynin as a strong anticholinergic. We stopped it. Within two weeks, she was back to herself. Her doctor had no idea it was the cause.” The FDA recorded over 1,200 cognitive-related adverse events in seniors from 2018 to 2022. Confusion was the most common. Memory loss came second. Delirium-sudden, severe mental confusion-was third. And here’s the kicker: 63% of older adults surveyed by the National Council on Aging said they were never told about the cognitive risks when these drugs were prescribed. Most assumed the doctor had checked for safety. They didn’t know they were being given a silent threat.What Can Be Done?
The good news? This is one of the few dementia risk factors we can actually change. The American Geriatrics Society’s 2023 Beers Criteria says: avoid strong anticholinergics in older adults. Period. And there are alternatives.- For allergies: Use non-sedating antihistamines like loratadine or cetirizine. They don’t cross into the brain.
- For overactive bladder: Mirabegron (Myrbetriq) works differently-no anticholinergic effect. Pelvic floor therapy is also effective.
- For depression: SSRIs like sertraline or escitalopram have little to no anticholinergic activity.
- For sleep: Melatonin or cognitive behavioral therapy for insomnia (CBT-I) are safer than diphenhydramine.
What Should Seniors and Families Do?
You don’t need to stop meds cold turkey. But you do need to ask questions.- Ask your doctor or pharmacist: “Is this medication anticholinergic? What’s the risk to my memory?”
- Ask: “Is there a non-anticholinergic alternative?”
- If you’ve been on a drug like oxybutynin or diphenhydramine for more than a year, ask about tapering it off.
- Keep a full list of all medications-including OTC and supplements-and bring it to every appointment.
- If you notice sudden confusion, forgetfulness, or trouble focusing after starting a new med, talk to your doctor immediately.
What’s Next?
The National Institute on Aging is funding a major study called CHIME, launching in 2024, to test whether actively reducing anticholinergic burden can delay or prevent cognitive decline in 3,500 seniors. Results are expected by 2027. Meanwhile, pharmaceutical companies are responding. Johnson & Johnson stopped making long-acting oxybutynin in 2021. Pfizer’s solifenacin, with less brain penetration, now holds over 20% of the bladder drug market. The European Medicines Agency and FDA have both updated warnings on anticholinergic labels. But warnings mean little if patients don’t understand them. The real change will come when doctors, pharmacists, and families start asking the same question: “Could this pill be hurting my brain?”Can anticholinergic drugs cause permanent brain damage?
Not always, but long-term use can lead to lasting changes. Brain imaging shows accelerated shrinkage and reduced metabolic activity in key memory areas. Some cognitive improvements occur after stopping the drugs-especially within the first 3 to 6 months-but full recovery isn’t guaranteed. The earlier you stop, the better the chance of reversing damage.
Is it safe to stop anticholinergic meds on my own?
No. Stopping suddenly can cause withdrawal symptoms like increased heart rate, sweating, or worsening of the original condition. Always work with your doctor to taper off safely. For example, stopping oxybutynin too fast can cause urinary retention. A slow reduction over 4 to 8 weeks is usually recommended.
Are over-the-counter sleep aids like Benadryl dangerous for seniors?
Yes. Diphenhydramine (Benadryl) is a Level 3 anticholinergic-strongly linked to confusion and memory loss in older adults. It’s one of the most common causes of preventable cognitive decline. Safer options include melatonin, magnesium, or cognitive behavioral therapy for insomnia (CBT-I).
Do all anticholinergic drugs affect the brain the same way?
No. Some drugs, like oxybutynin and diphenhydramine, easily cross into the brain and have strong effects. Others, like solifenacin or loratadine, are designed to stay outside the brain and have minimal or no cognitive impact. The ACB scale helps distinguish between them.
Can I reduce my anticholinergic burden if I’m on multiple meds?
Absolutely. Start by listing every medication, including vitamins and OTC drugs. Bring it to your doctor or pharmacist and ask for an ACB score calculation. Often, one or two drugs can be replaced with safer alternatives. Even reducing your total ACB score from 4 to 2 can lower your dementia risk significantly.
Why don’t doctors always know about anticholinergic risks?
Many were trained before these risks were fully understood. Also, most doctors focus on treating the immediate condition-like bladder urgency or depression-without considering long-term brain effects. The 2023 Beers Criteria changed that, but awareness still lags behind evidence. Asking the question helps push change.