Understanding Asthma and Chronic Sinusitis
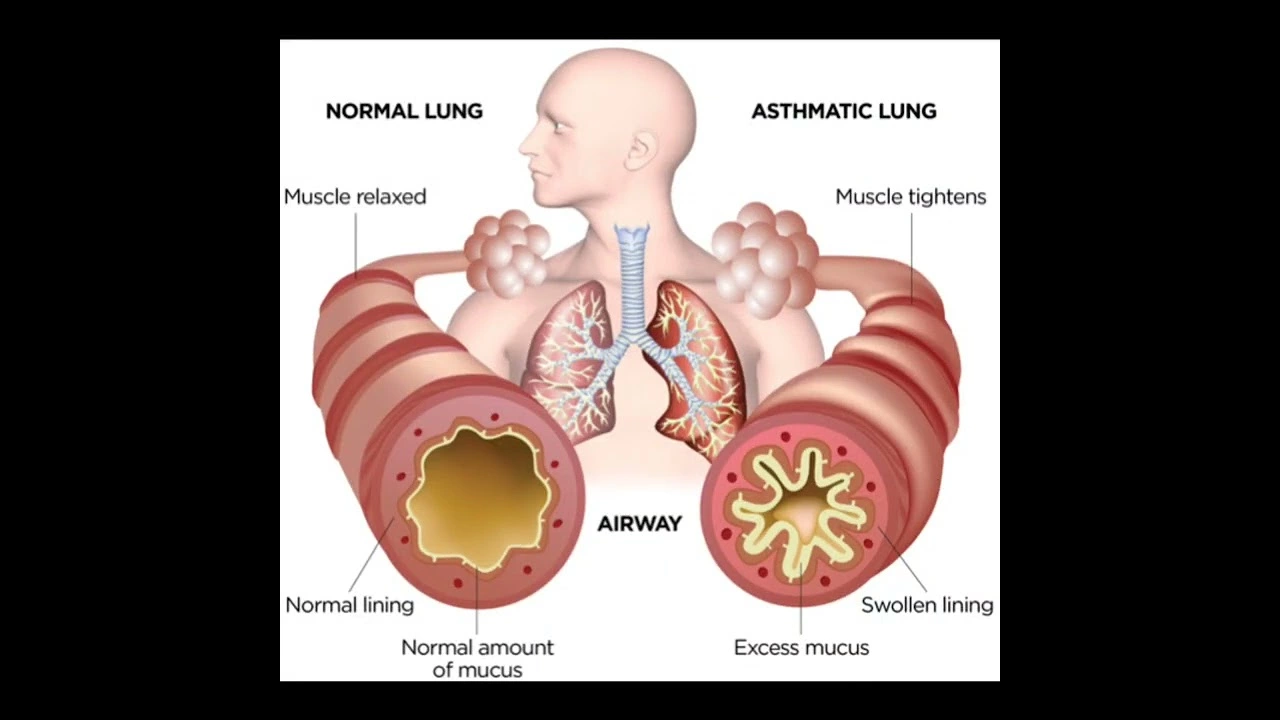
Before we dive into the connection between asthma and chronic sinusitis, it's crucial to understand what these conditions are. Asthma is a long-term inflammatory disease that affects the airways of the lungs. It is characterized by recurrent episodes of wheezing, shortness of breath, chest tightness, and coughing. On the other hand, chronic sinusitis is a common condition where the spaces inside your nose and head (sinuses) are swollen and inflamed for three months or longer, despite treatment attempts. This condition interferes with drainage and causes mucus to build up, leading to difficulties breathing through the nose.
Common Symptoms of Asthma and Chronic Sinusitis
Although asthma and sinusitis are separate conditions, they share some common symptoms. These include shortness of breath, wheezing, and coughing. With chronic sinusitis, you may also experience nasal congestion, facial pain, or reduced sense of smell and taste. The overlap of symptoms can sometimes make it challenging to determine whether you're experiencing an asthma attack or a sinusitis flare-up.
The Link Between Asthma and Chronic Sinusitis
Research has shown that there is a significant link between asthma and chronic sinusitis. Both conditions involve inflammation and swelling of the airways, which can lead to difficulty breathing. Furthermore, chronic sinusitis can often trigger asthma attacks, making it a common comorbidity in individuals with asthma. The reason for this connection is still being researched, but it's believed that the inflammation caused by sinusitis can spread to the lungs, triggering asthma symptoms.
Impact of Sinusitis on Asthma Control
Chronic sinusitis can significantly impact the control and management of asthma. It can cause an increase in asthma symptoms and attacks, leading to more frequent use of medication. Moreover, individuals with both conditions may find that their asthma symptoms are more severe and harder to control.
Diagnosis of Asthma and Chronic Sinusitis
Given the connection between asthma and sinusitis, it's crucial for healthcare providers to accurately diagnose and treat these conditions. Diagnosis typically involves a physical examination, review of medical history, and specific tests, such as breathing tests for asthma and imaging tests for sinusitis. Prompt and accurate diagnosis can lead to more effective treatment and better management of symptoms.
Treatment Options for Asthma and Sinusitis
While there's no cure for either asthma or chronic sinusitis, treatments can help manage symptoms and prevent complications. Asthma treatments often involve long-term control medications and quick-relief (rescue) inhalers. For chronic sinusitis, treatments may include nasal corticosteroids, saline nasal irrigation, or in some severe cases, surgery.
Preventing Asthma Attacks Triggered by Sinusitis
Preventing sinusitis flare-ups can be an effective way to reduce the frequency and severity of asthma attacks. This can be achieved through various measures such as avoiding known triggers, maintaining good sinus hygiene, and staying up-to-date with immunizations.
Living with Asthma and Chronic Sinusitis
Living with both asthma and chronic sinusitis can be challenging, but it's manageable with the right care and treatment plan. It's essential to work closely with your healthcare provider to manage your symptoms effectively and maintain a good quality of life.
The Importance of Regular Check-ups
Regular check-ups are vital in managing both asthma and chronic sinusitis. These allow your healthcare provider to monitor your condition, adjust your treatment plan as needed, and prevent potential complications. It's crucial to make sure you attend these appointments and communicate any changes in your symptoms to your healthcare provider.
Conclusion: Taking Control of Your Health
In conclusion, while the connection between asthma and chronic sinusitis can complicate the management of these conditions, it's essential to remember that you have the power to take control of your health. By understanding your conditions, working closely with your healthcare provider, and taking proactive steps to manage your symptoms, you can live a healthy, active life.

lata Kide
July 7, 2023 AT 05:20Wow, the link between asthma attacks and chronic sinusitis is like a dramatic soap‑opera inside our bodies! 🌟 I’ve been battling both for years, and let me tell you, the constant wheezing and that relentless sinus pressure feel like a never‑ending cliffhanger. 😱 Did you know that the inflammation can travel from your nose down to your lungs, basically turning a simple sneeze into a full‑blown asthma episode? 🤧 Trust me, I’ve read *everything* on the topic, from obscure journals to midnight health blogs, and the evidence is screaming louder than a siren. 🚨 So, if you’re feeling the squeeze, remember you’re not alone – we’re all starring in this respiratory drama together! 🎭
Mark Eddinger
July 7, 2023 AT 05:28Thank you for sharing your experience. The pathophysiology described aligns with current literature, which indicates that nasal inflammation can exacerbate lower airway hyper‑responsiveness. Proper management typically involves a combination of inhaled corticosteroids for asthma and nasal saline irrigation or intranasal steroids for sinusitis. Regular monitoring and coordinated treatment plans are essential to reduce the frequency of exacerbations. Should you require further clarification, peer‑reviewed sources such as the American Thoracic Society guidelines provide comprehensive recommendations.
Francisco Garcia
July 7, 2023 AT 05:40I appreciate the thorough overview and would add that environmental factors, such as allergens and air quality, often play a pivotal role in both conditions. In many cultures, especially where indoor heating is prevalent, patients report seasonal spikes in symptoms. Collaborative care that includes allergen avoidance, immunotherapy, and patient education can substantially improve outcomes. Moreover, sharing personal stories, like the one you mentioned, helps clinicians understand the real‑world impact of these intertwined diseases.
Patrick Renneker
July 7, 2023 AT 06:10While the prevailing consensus posits a direct causal relationship between chronic sinusitis and asthma exacerbations, a meticulous examination of the extant data reveals several methodological shortcomings that warrant cautious interpretation. First, many of the cited studies suffer from selection bias, enrolling patients already predisposed to respiratory ailments, thereby inflating the apparent association. Second, the heterogeneity of diagnostic criteria across investigations renders cross‑study comparisons precarious, as sinusitis severity is often categorized arbitrarily. Third, the inflammatory mediators implicated in sinus pathology, such as interleukin‑5 and eosinophilic cationic protein, are not uniquely predictive of lower airway involvement, suggesting that correlation does not equate to causation. Fourth, longitudinal trials that have employed rigorous randomization protocols have failed to demonstrate a statistically significant reduction in asthma attacks following sinusitis‑targeted therapies. Fifth, the influence of confounding variables-including smoking status, occupational exposures, and concomitant allergic rhinitis-has been inconsistently adjusted for in multivariate analyses. Sixth, the reliance on patient‑reported outcome measures introduces an element of subjectivity that may exaggerate perceived symptom overlap. Seventh, recent meta‑analyses have highlighted a disparity between symptom improvement and measurable changes in pulmonary function tests, underscoring a potential placebo effect. Eighth, the advent of biologic agents that modulate type‑2 inflammation has further complicated the narrative, as these therapies simultaneously address both sinus and airway disease, obscuring the directionality of benefit. Ninth, animal models designed to elucidate mechanistic pathways often employ artificial induction methods that do not faithfully replicate human disease processes. Tenth, the economic incentives inherent in pharmaceutical research may bias the dissemination of favorable findings, thereby skewing the literature. Eleventh, geographical variations in microbiome composition suggest that regional factors could modulate disease interaction, a dimension largely overlooked in current studies. Twelfth, the potential role of chronic viral infections, which can inhabit both sinus and bronchial tissues, remains an underexplored confounder. Thirteenth, the impact of surgical interventions, such as functional endoscopic sinus surgery, on long‑term asthma control has yielded mixed results, with some cohorts reporting no appreciable benefit. Fourteenth, patient adherence to prescribed regimens, both for asthma and sinusitis, is notoriously variable and can significantly influence clinical outcomes. Finally, it remains prudent to acknowledge that while a bidirectional relationship is plausible, the evidence supporting a deterministic link is, at best, equivocal, and further high‑quality, prospective research is indispensable before definitive clinical guidelines can be established.
KAYLEE MCDONALD
July 7, 2023 AT 06:18Even if the link is fuzzy, patients still need clear, assertive treatment plans.
Alec McCoy
July 7, 2023 AT 06:43Hey everyone, let’s take this conversation a step further and focus on actionable steps you can incorporate today. First, keep a symptom diary – note when your nasal congestion spikes and whether you notice a corresponding dip in your breathing ease. Second, try nasal irrigation twice daily; it’s a simple habit that can flush out irritants and reduce inflammation. Third, don’t underestimate the power of a well‑timed inhaled corticosteroid dose before known triggers, like pollen season or dust exposure. Fourth, consider consulting an ENT specialist about possible sinus CT imaging, especially if you haven’t had one in the past few years. Fifth, stay proactive with your primary care provider: review your asthma action plan quarterly and adjust medications based on recent lung function tests. Remember, managing both conditions isn’t a solo battle; lean on your healthcare team, ask questions, and celebrate the small victories – each breath taken with less effort is a win!
Aaron Perez
July 7, 2023 AT 06:53Indeed; the pursuit of respiratory harmony evokes a timeless philosophical quandary – does the body seek equilibrium, or does equilibrium dictate the body? One might argue that the sinus passages, like the corridors of an ancient library, house secrets that echo within the bronchial chambers; yet, the very act of breathing transforms these whispers into a symphony of life. It is essential, therefore, to recognize that treatment is not merely a mechanistic protocol, but a dialogue between organism and environment; a dialogue that demands both rigor and humility. Caution must be exercised, lest we impose a rigid regimen that smothers the innate adaptability inherent in our physiology. In this light, the integration of mindful breathing practices, coupled with evidence‑based medication, forms a balanced approach that honors both science and the subtle art of self‑regulation.