Hepatic encephalopathy: what to watch for and what helps
Hepatic encephalopathy (HE) happens when a damaged liver can’t clear toxins and those toxins affect the brain. If you or someone you care for has liver disease, HE is one of the serious problems to recognize early. This page gives clear, actionable info on common triggers, how it looks, and practical treatments that doctors use every day.
How HE starts and common triggers
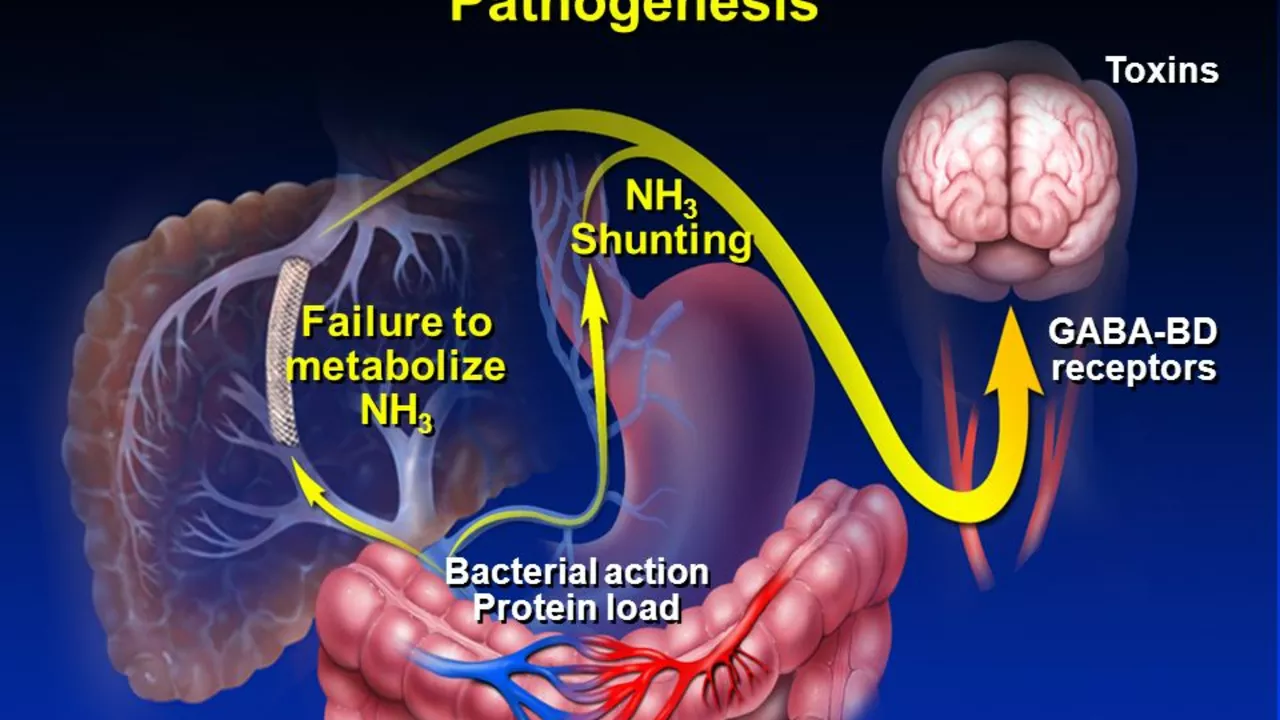
The basic issue is build-up of toxins like ammonia that the liver normally removes. HE often appears in people with cirrhosis or after major liver injury. Common triggers you can watch for include infections, GI bleeding, constipation, dehydration, changing medicines (especially sedatives or opioids), and electrolyte imbalances. Even simple things like missing dialysis or eating a heavy protein meal can tip someone into symptoms.
Signs, from subtle to severe
Symptoms range from mild to life‑threatening. Mild signs: confusion, trouble concentrating, sleep pattern change, mood swings. Look for subtle personality shifts that family members notice first. Moderate signs: slurred speech, slowed movements, obvious confusion. Severe HE: stupor, inability to respond, coma. A classic physical sign is a flapping tremor of the hands called asterixis — if you see that, get urgent care.
Doctors use the history and exam first. Lab tests often show high ammonia, but ammonia levels don’t always match how sick someone looks. EEG (brain tracing) can help in unclear cases. Imaging rules out other causes like stroke. Most important is spotting and treating the trigger early.
Treatment focuses on two goals: remove or treat the trigger, and lower toxin production. For toxin control, the standard starting medicine is lactulose — a sugar solution you drink or get by enema. It helps push ammonia out by changing gut bacteria and stool consistency. If lactulose alone isn’t enough, doctors add rifaximin, a non-absorbed antibiotic that lowers ammonia-producing gut bugs. Treat infections, control bleeding, correct electrolytes, and stop sedating meds when possible.
For people who’ve had repeated episodes, maintenance therapy with lactulose (and sometimes rifaximin) reduces recurrences. Nutritional advice matters: avoid prolonged fasting and keep a steady, adequate protein intake—protein restriction is usually harmful long term. Work with a liver specialist or dietitian for a plan that fits your case.
When should you get emergency help? Any sudden confusion, severe drowsiness, vomiting blood, or breathing problems needs emergency care. HE can progress fast; earlier treatment often prevents hospital stays and complications.
Living with HE means managing liver disease, keeping up with medications, watching for triggers, and having a clear plan for urgent care. Talk openly with your care team about symptom warning signs and when to call. With prompt action and the right meds, many people stabilize and avoid repeated crises.
The Connection Between Hepatic Encephalopathy and Muscle Weakness
Alright folks, today we're diving into a pretty heavy topic - the link between Hepatic Encephalopathy (let's call it HE for simplicity's sake) and muscle weakness. Now, don't let those big words scare you, it's simpler than it sounds! HE, a condition that affects your brain when your liver can't remove toxins, has been found to have a surprising relationship with muscle weakness. Imagine your muscles throwing a party and then HE comes uninvited, causing quite a ruckus! So, next time you're feeling a bit weak in the knees, don't panic, but maybe give your liver some love, it might just be dealing with some unwanted guests.
Read moreHepatic Encephalopathy: The Difference Between Acute and Chronic Cases
In my recent study, I delved into Hepatic Encephalopathy, a serious condition that affects the brain due to liver disease. I learned that it comes in two forms: acute and chronic. Acute cases are sudden, severe, and often associated with a specific trigger like an infection or the use of certain medications. On the other hand, chronic cases develop slowly over time, often due to long-standing liver disease or cirrhosis. It's crucial to understand these differences, as both types require different approaches in management and treatment.
Read more